I have seen a fair few patients that I have diagnosed with pericarditis. It seems that I've probably over-diagnosed it in quite a lot of people! 5% of patients presenting to the ED with non-ischaemic chest pain have acute pericarditis - so my numbers are probably right.
The Pain
- Relieved by leaning forward
- Can radiate to the trapezius ridge as the phrenic nerve travels
Signs
- Pericardial friction rub in 85% of cases
- Rub still heard on breath holding
ECG
- Diffuse concave or saddle shaped ST changes, with ST elevation in 90% of cases, typically leads Ι, ΙΙ, V5 and V6
- Associated ST depression in aVR and V1 is seen in 64% of cases [6].
- PR depression
- Look carefuly at V6. If ST elevation to T wave height ratio is greater than 0.25, acute pericarditis is more likely than BER.
Diagnosis - needs 2/4
Characteristic chest pain
Pericardial friction rub
Suggestive ECG changes
New or worsening pericardial effusion
High Risk features
Temperature greater than 38ºC
Raised WCC
Large pericardial effusion
Cardiac tamponade
Acute trauma
Immunosuppression
Oral anticoagulants
Failure of NSAID therapy
Recurrent pericarditis
Troponin levels are elevated in 30-70% of patients with 'pericarditis'; they offer no prognostic information.
Pericardial Effusion
A true diagnosis needs relief of symptoms from pericardiocentesis.
Signs - Pulsus paradoxus is an exaggerated fall in systolic blood pressure of 10 mmHg or more during inspiration.
The Beck triad is present in only a minority of patients
References
http://sinaiem.org/cardiac-tamponade/
https://radiopaedia.org/articles/cardiac-tamponade
http://www.rcemlearning.co.uk/modules/acute-pericarditis/ http://www.rcemlearning.co.uk/references/pericarditis/
https://coreem.net/core/pericarditis/
http://www.emnote.org/emnotes/ecg-findings-of-pericarditis
Monday 26 December 2016
Wednesday 2 November 2016
Management Part 5 - general
Your Department Overview
You are always likely to be the lead
Notice the dates
Look at how many Consultants there are in the department and if this is right for CEM guidance
Prepare a one liner about the department eg TU med
Always then do a shift walk / speak to SpR / NIC
Comment on anything that is abnormal
If you are running late, ask the day registrar to ring the night registrar
If you delegate say you will be available all the time so anyone can work under my direct supervision
Always signpost your diary - say I will deal with the urgent things first...
Always be prepared to cancel things in your diary eg. the drains if there's a majax
Don't say juniors - say medical or nursing staff
Content
If there's targets, look at how far through the year we are and how close to target we are
If there's name and shame state this is a dysfunctional department
If there's audits, look at who does the audit
If they mention patient details, do you have enough identifiers?
Emails
Look at who they came from and when
The CEO is automatically important
Always look at who is CC'd
Bring in comissioning
Rules
You can't discipline Nurses
Matron can't discipline medics
FY2 teaching
Look at who is staffing the department
Reference Request
We must have known for 36 months
Find out who was supervisor
Review appraisals
Assume it was you that you were their supervisor
Give an accurate reference
Incident Forms
Say that all incident forms will be appropriately assigned. From this report, it would not be assigned to me but if it was... ...
Teaching
Always mention teaching - mention the teaching programme/ induction. If the FY2s are at teaching, who is running the department.
Look at the topics - if there is something like "foolish mistakes by patients" state that this is degrading.
Late Night Swaps
State it is against policy
But that you would try to help
Remind people on induction of the policy, and resend policy.
Forging Signatures
Locum agency to investigate
?Signature record with the secretaries
Say the locum isn't coming back
Medication Shortage
Shortage does not = gone
Can we stockpile
Keep pharmacy link in the loop
Email / poster in the back of the loo
Tell Nurses there is a shortage
Physically stick the sign in the resus cupboard
Bomb Threat
Gather some information - is it real?
Escalate to all co-located services - NIC, duty manager.
State there is a policy
Police liason officer
Doctor being bullyed
SUI
Bullying policy
Phone the doctor
Time of shift swapping
Having worked with these 2 FY2s I will have an awareness of their characteristics...
Sisters is a Nursing Issue
Get a copy of the notes, add my notes. Store in "incidents file"
Saturday 22 October 2016
Fascia Iliaca Blocks
Fascia Iliaca blocks are really useful for analgesia for hip fractures. We should be performing them!
Fascia Iliaca or Femoral?
My understanding of this is if we're using a landmark approach, and we use a femoral nerve block the risk of not being in the right soft tissue plane is high. This means that a fascia iliaca block us more likely to be beneficial. The evidence, which I haven't appraised myself, suggests that there's not a significant amount of difference between them all.
Anatomy
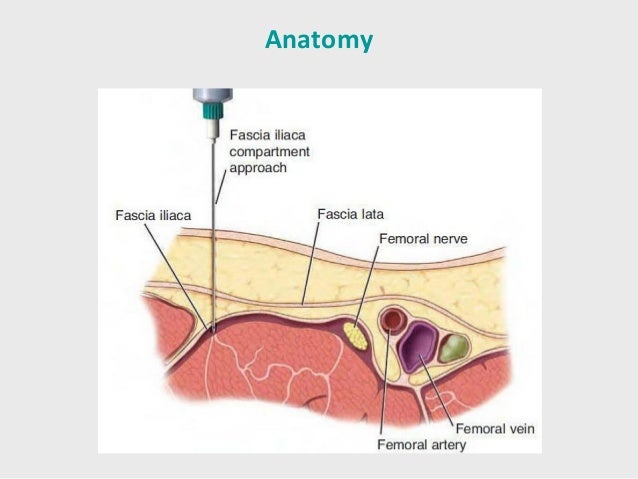
If you look here you can see that the femoral nerve sits, and is enclosed between the fascia lata and the facia iliaca. If you go just lateral to it, you don't know whether you are above or below the fascia iliaca. If you do a fascia iliaca compartment approach, you know you are in the right space.
The podcast from Anatomy for EM is excellent at running through this.
The fascia iliaca compartment contains the three main nerves we are interested in blocking - the femoral nerve, lateral femoral cutaneous and obterator. They provide analgesia for all of the leg except the posterior bit - which the sciatic nerve covers.
Contraindications
· Patient refusal
· Anticoagulation
· Previous femoral bypass surgery
· Inflammation or infection over injection site
· Allergy to local anaesthetics
· Previous femoral bypass surgery
Anaesthetic
We need to use large amounts of local anaesthetic to perform this. 30-40ml should be used for every adult sized patient, and anaesthetic adjusted accordingly.
Our maximum doses are:
Bupivacaine 2mg/kg
Lidocaine 3mg/kg
We normal use 0.25% bupivacaine to provide maximum volume. For a 80kg patient, this would be 160mg which is 60ml of 0.25% bupivacaine. Which is quite a lot. Bupivacaine often works slowly but lasts for a while.
Landmarks
Place one middle finger on the ASIS and the other middle finger on the pubic tubercle.
Draw a line between these two points.
Divide this line into thirds.
Mark the point 1 - 2 cm caudal from the junction of the lateral and middle third.
This is where you are aiming for.
Ultrasound
Ultrasound for blocks isn't yet common practice. I use it to help avoid accidental intravascular injection - put the probe on where I'm going to inject, and double check.
You can see the two fascial layers on ultrasound, and see the local anaesthetic expand. This video demonstrates the use of ultrasound wonderfully.
Complications
Failure
Infection
Accidental intravascular or intraneural injection
Local anaesthetic toxicity
Links and References
http://www.propofology.com/infographs/fascia-iliaca-block
http://learned.rocks/cooked-resourced/2016/8/15/nerve-blocks
http://www.rcemlearning.co.uk/modules/fascia-iliaca-block/
https://songsorstories.com/2016/07/31/pop-pop-phew-sounds-to-go-with-blocks/
http://www.thegasmanhandbook.co.uk/fascia-iliaca-block.html
http://stemlynsblog.org/fib-virgil/
http://bestbets.org/bets/bet.php?id=2673
Fascia Iliaca or Femoral?
My understanding of this is if we're using a landmark approach, and we use a femoral nerve block the risk of not being in the right soft tissue plane is high. This means that a fascia iliaca block us more likely to be beneficial. The evidence, which I haven't appraised myself, suggests that there's not a significant amount of difference between them all.
Anatomy
If you look here you can see that the femoral nerve sits, and is enclosed between the fascia lata and the facia iliaca. If you go just lateral to it, you don't know whether you are above or below the fascia iliaca. If you do a fascia iliaca compartment approach, you know you are in the right space.
The podcast from Anatomy for EM is excellent at running through this.
The fascia iliaca compartment contains the three main nerves we are interested in blocking - the femoral nerve, lateral femoral cutaneous and obterator. They provide analgesia for all of the leg except the posterior bit - which the sciatic nerve covers.
Contraindications
· Patient refusal
· Anticoagulation
· Previous femoral bypass surgery
· Inflammation or infection over injection site
· Allergy to local anaesthetics
· Previous femoral bypass surgery
Anaesthetic
We need to use large amounts of local anaesthetic to perform this. 30-40ml should be used for every adult sized patient, and anaesthetic adjusted accordingly.
Our maximum doses are:
Bupivacaine 2mg/kg
Lidocaine 3mg/kg
We normal use 0.25% bupivacaine to provide maximum volume. For a 80kg patient, this would be 160mg which is 60ml of 0.25% bupivacaine. Which is quite a lot. Bupivacaine often works slowly but lasts for a while.
Landmarks
Place one middle finger on the ASIS and the other middle finger on the pubic tubercle.
Draw a line between these two points.
Divide this line into thirds.
Mark the point 1 - 2 cm caudal from the junction of the lateral and middle third.
This is where you are aiming for.
Ultrasound
Ultrasound for blocks isn't yet common practice. I use it to help avoid accidental intravascular injection - put the probe on where I'm going to inject, and double check.
You can see the two fascial layers on ultrasound, and see the local anaesthetic expand. This video demonstrates the use of ultrasound wonderfully.
Complications
Failure
Infection
Accidental intravascular or intraneural injection
Local anaesthetic toxicity
Links and References
http://www.propofology.com/infographs/fascia-iliaca-block
http://learned.rocks/cooked-resourced/2016/8/15/nerve-blocks
http://www.rcemlearning.co.uk/modules/fascia-iliaca-block/
https://songsorstories.com/2016/07/31/pop-pop-phew-sounds-to-go-with-blocks/
http://www.thegasmanhandbook.co.uk/fascia-iliaca-block.html
http://stemlynsblog.org/fib-virgil/
http://bestbets.org/bets/bet.php?id=2673
Thursday 13 October 2016
Management part 4 - Complaints
Complaints are unfortunately comment and cost the NHS a lot in time to investigate, and litigation costs. GMC guidance says patients are allowed to complain, and their complaints must be investigated and not bias the care they are provided.
Formal complaints must be made within six months of the event, or the patient becoming aware of the event up to a maximum of a year of the event, by the patient or relative.
The trust has 3 days to acknowledge the complaint, and 25 working days to reply with a response (10 days in primary care).
Always mention PALS
There are three types of claim:
•Category A Claims: below which the trust bears the costs of any settlement (eg £20 000-250000).
•Category B Claims: claims over and above this are settled by the CNST in part (20%)
•Category C Claims: above this threshold (£500 000) settlement paid in full by CNST
To exist, medical negligence requires:
- Duty of care existed
- Duty was breached (Bolam/Bolitho tests)
- Harm occurred as a result of the breach
To get compensation, a patient needs to prove:
That the treatment fell below a minimum standard of competence; and
That he/she has suffered an injury; and
That it is more likely than not that the injury would have been avoided, or less severe, with proper
treatment
2) Being customer focused
3) Being open and accountable
4) Acting fairly and proportionately
5) Putting things right
6) Seeking continuous improvement
When dealing with a complainant, the 3 Rs can be helpful.
Regret
Reason
Remedy
Complaints from GPs
This is not a complaint it's colleague to colleague
Can ring the emailer back, acknowledge mistake, praise their system and make it positive ?audit
Involve GPs in plans/ audit
Local resolution
Datix
http://michael.gradmedic.org/medicine/medicolegal.html#negligence
http://fcemprep.blogspot.co.uk/2014/09/the-fcem-management-viva-basics.html?m=1
Formal complaints must be made within six months of the event, or the patient becoming aware of the event up to a maximum of a year of the event, by the patient or relative.
The trust has 3 days to acknowledge the complaint, and 25 working days to reply with a response (10 days in primary care).
Always mention PALS
There are three types of claim:
•Category A Claims: below which the trust bears the costs of any settlement (eg £20 000-250000).
•Category B Claims: claims over and above this are settled by the CNST in part (20%)
•Category C Claims: above this threshold (£500 000) settlement paid in full by CNST
To exist, medical negligence requires:
- Duty of care existed
- Duty was breached (Bolam/Bolitho tests)
- Harm occurred as a result of the breach
To get compensation, a patient needs to prove:
That the treatment fell below a minimum standard of competence; and
That he/she has suffered an injury; and
That it is more likely than not that the injury would have been avoided, or less severe, with proper
treatment
There are six main components of good complaints handling.
1) Getting it right2) Being customer focused
3) Being open and accountable
4) Acting fairly and proportionately
5) Putting things right
6) Seeking continuous improvement
When dealing with a complainant, the 3 Rs can be helpful.
Regret
Reason
Remedy
Complaints from GPs
This is not a complaint it's colleague to colleague
Can ring the emailer back, acknowledge mistake, praise their system and make it positive ?audit
Involve GPs in plans/ audit
Local resolution
Datix
http://michael.gradmedic.org/medicine/medicolegal.html#negligence
http://fcemprep.blogspot.co.uk/2014/09/the-fcem-management-viva-basics.html?m=1
Friday 7 October 2016
Management Part Two - Disciplinary and Policies
· Warnings
· Verbal
· Written
· HR issues
• Grievance is an ‘Employee’s complaint’ against management.
• Discipline is a ‘Management’s complaint’ against an employee.
Clinical Issues
- Follow Trainee in Difficulty advice
- NCAS involvement may be necessary
- An informal route may be decided on
Retraining, re-skilling, e.g. workshops, e-learning,
Counselling, rehabilitation, e.g. NHS Practitioner Health Programme
Supervision or development support programme e.g. supervised practice, formative work-based assessments
Mentoring or coaching, career guidance
- If needs investigating medical director appoints case investigator.
- Complete within four weeks
- If need formal capability hearing, need 20 days notice, 2 members of trust board and one practitioner from outside the Trust. Advice from HR, senior Clinician from outside the trust.
- Outcomes could be agreement for improvement, formal written warning, final written warning or dismissal. Dismissal needs to be reported to the GMC.
Referral to the GMC
If:
a. The doctor’s ill health is posing, or may pose, a risk to patients;
b. The doctor refuses, or has failed, to follow advice and guidance from his or her own doctor, occupational health adviser or employer.
c. The doctor’s conduct has led to the involvement of the police and/or the courts or raised other concerns.
Holiday Leave
The annual entitlement under Agenda for Change for each full-time member of staff is:
On appointment 27 days + 8 General Public Holidays
After 5 years service 29 days + 8 General Public Holidays
After 10 years service 33 days + 8 General Public Holidays
Whistleblowing
If concerns speak to CD. If still have concerns anyone can speak to the board.
Management - performance related issues
The FRCEM has a whole management viva. Here are some of my notes on some of the common themes.
• Working practices
• Competencies’
• Team work
• Reliability
• Guidelines / pathways
• Lack of insight
• Sickness
• Probity
• Difficult colleagues / colleagues in difficulty
Speed
Check the numbers before you speak to people about it - facts often don't reflect reality.
Trainee in Difficulty
a nationally accepted phrase used to describe:
a doctor or dentist on a postgraduate training programme, who for whatever reason, needs extra help and support - beyond that which is normally required - to deal with an issue, or issues, that threaten to impede their progress towards completion of a postgraduate training programme
The purpose of identifying a trainee as being “in difficulty” is not to label them; it is to aid the addressing of relevant issues so that they may complete training successfully and continue to contribute to the work of the NHS.
Doctor in difficulty recognises that it’s not just trainees that might be in difficulty – TID is the new term.
If a problem happens, your role initially is not to investigate. You need to ensure safety of:
The patient – go and review them
The staff – support the SHO
Support the SpR and decide if this is a doctor in difficulty.
10 Signs of a Doctor in Difficulty
- The “disappearing act” - disappearing; lateness; frequent sick leave.
- Low work rate - leaving late and still not achieving a reasonable workload.
- Ward rage - bursts of temper; shouting matches; real or imagined slights
- Rigidity - poor tolerance of ambiguity; inability to compromise; difficulty prioritising; inappropriate ‘whistle blowing’.
- Bypass syndrome - junior colleagues or nurses find ways to avoid seeking the doctor’s opinion or help
- Career problems - difficulty with exams; uncertainty about career choice; disillusionment with medicine
- Insight failure - rejection of constructive criticism; defensiveness; counter-challenge.
- Lack of engagement in educational processes - fails to arrange appraisals, late with learning events/workbased assessments, reluctant to complete portfolio, little reflection
- Lack of initiative/appropriate professional engagement
the trainee may come from a culture where there is a rigid hierarchical structure and trainees are not encouraged to question patient management decisions by senior colleagues, or demonstrate other healthy assertive behaviours
- Inappropriate attitudes
The cultural background may be very strongly male oriented and the trainees may not be used to working with females on an equal status basis
From isolated incidents it is often difficult to know. It is important to report incidents if and when they happen so pattern can be identified.
Causes
Clinical Performance - capability and learning
Health - physical and mental
Personality and Behaviour
Environment - home and work
Management
Early identification of problems
Establish and clarify the facts, with as many sources of information as possible.
Poor performance is a symptom and not a diagnosis.
Clear documentation
Communicate misgivings. Complete records. Remedies must be sought. Progression must be delayed until issues resolved.
Patient safety greater than all
Remain focused on specific problem
Refrain from generalised comment
Deal with the specific behaviour
Try to find positive
Avoid ‘You’ and use ‘I’
Explain how you think
Wait
If facing hostility, state their feelings
Avoid confrontation
Use empathic assertion
Active listening
Control anger
Let their anger subside
When to refer to the GMC
If the Drs illness is impacting his or her performance, and one or more of:
Drs ill health is posing, or may pose, a risk to patients
Dr refuses or has failed to follow advice and guidance from his or her own patients, occy health or employer.
Drs conduct has lead to the involvement of the police/ and or the courts or raised other concerns.
Discuss potential referrals with GMC or NCAS first.
References
http://stemlynsblog.org/overconfidence-in-the-ed/
• Working practices
• Competencies’
• Team work
• Reliability
• Guidelines / pathways
• Lack of insight
• Sickness
• Probity
• Difficult colleagues / colleagues in difficulty
Speed
Check the numbers before you speak to people about it - facts often don't reflect reality.
Trainee in Difficulty
a nationally accepted phrase used to describe:
a doctor or dentist on a postgraduate training programme, who for whatever reason, needs extra help and support - beyond that which is normally required - to deal with an issue, or issues, that threaten to impede their progress towards completion of a postgraduate training programme
The purpose of identifying a trainee as being “in difficulty” is not to label them; it is to aid the addressing of relevant issues so that they may complete training successfully and continue to contribute to the work of the NHS.
Doctor in difficulty recognises that it’s not just trainees that might be in difficulty – TID is the new term.
If a problem happens, your role initially is not to investigate. You need to ensure safety of:
The patient – go and review them
The staff – support the SHO
Support the SpR and decide if this is a doctor in difficulty.
10 Signs of a Doctor in Difficulty
- The “disappearing act” - disappearing; lateness; frequent sick leave.
- Low work rate - leaving late and still not achieving a reasonable workload.
- Ward rage - bursts of temper; shouting matches; real or imagined slights
- Rigidity - poor tolerance of ambiguity; inability to compromise; difficulty prioritising; inappropriate ‘whistle blowing’.
- Bypass syndrome - junior colleagues or nurses find ways to avoid seeking the doctor’s opinion or help
- Career problems - difficulty with exams; uncertainty about career choice; disillusionment with medicine
- Insight failure - rejection of constructive criticism; defensiveness; counter-challenge.
- Lack of engagement in educational processes - fails to arrange appraisals, late with learning events/workbased assessments, reluctant to complete portfolio, little reflection
- Lack of initiative/appropriate professional engagement
the trainee may come from a culture where there is a rigid hierarchical structure and trainees are not encouraged to question patient management decisions by senior colleagues, or demonstrate other healthy assertive behaviours
- Inappropriate attitudes
The cultural background may be very strongly male oriented and the trainees may not be used to working with females on an equal status basis
From isolated incidents it is often difficult to know. It is important to report incidents if and when they happen so pattern can be identified.
Causes
Clinical Performance - capability and learning
Health - physical and mental
Personality and Behaviour
Environment - home and work
Management
Early identification of problems
Establish and clarify the facts, with as many sources of information as possible.
Poor performance is a symptom and not a diagnosis.
Clear documentation
Communicate misgivings. Complete records. Remedies must be sought. Progression must be delayed until issues resolved.
Patient safety greater than all
Remain focused on specific problem
Refrain from generalised comment
Deal with the specific behaviour
Try to find positive
Avoid ‘You’ and use ‘I’
Explain how you think
Wait
If facing hostility, state their feelings
Avoid confrontation
Use empathic assertion
Active listening
Control anger
Let their anger subside
When to refer to the GMC
If the Drs illness is impacting his or her performance, and one or more of:
Drs ill health is posing, or may pose, a risk to patients
Dr refuses or has failed to follow advice and guidance from his or her own patients, occy health or employer.
Drs conduct has lead to the involvement of the police/ and or the courts or raised other concerns.
Discuss potential referrals with GMC or NCAS first.
http://stemlynsblog.org/overconfidence-in-the-ed/
Monday 26 September 2016
Back Examination
We do back pain examination every day, but it is worth remembering how to do it properly.
- Introduction, Consent, Handwashing, Chaparone. Exposure from the waist up
- Inspection
Inspection from the back and side for:
Cervical lordosis, thoracic kyphosis and lumbar lordosis (lost with age, ank spond, acute disc prolapse).
Cafe au lait spots (neurofibromatosis), hairy patch (spinal dysraphism)
Muscle wasting
Scars
- Palpation
For temperature
Palpate each spinous process
Palpate sacroiliac joints
Palpate paraspinal muscles
Percuss with a fist or tendon hammer (infection, fracture or tumour)
- Move
Lumbar: Lumbar flexion, extension and lateral flexion.
run hands down side (lateral flexion)
touch their toes with knees straight (flexion)
lean backwards with knes straight (extension) - no extension in facet disease.
Can do a modified Schobers Test - place index and middle fingers 5 centimeters apart and noting how close and far apart they move on the movements.
C-Spine
Lateral flexion: place your ear on your shoulder;
rotation: look over your shoulder;
flexion: put your chin on your chest;
extension: put your head back to look at the ceiling.
Thoracic
Fix pelvis and turn
- Special Tests
Straight leg raise - to look for sciatica
Sciatic nerve test - do SLR. When pain brought on, dorsiflex the foot = positive = sciatic!
Bowstring test - SLR. Then lower. Apply popliteal compression = symptoms.
Femoral nerve stretch test - lie prone, passively flex knee - severe = positive.
Tiptoe test - tests S1
Duck walk (on heels) - for L4 power
Neurological examination
References
http://www.osceskills.com/e-learning/subjects/spine-examination/
- Introduction, Consent, Handwashing, Chaparone. Exposure from the waist up
- Inspection
Inspection from the back and side for:
Cervical lordosis, thoracic kyphosis and lumbar lordosis (lost with age, ank spond, acute disc prolapse).
Cafe au lait spots (neurofibromatosis), hairy patch (spinal dysraphism)
Muscle wasting
Scars
- Palpation
For temperature
Palpate each spinous process
Palpate sacroiliac joints
Palpate paraspinal muscles
Percuss with a fist or tendon hammer (infection, fracture or tumour)
- Move
Lumbar: Lumbar flexion, extension and lateral flexion.
run hands down side (lateral flexion)
touch their toes with knees straight (flexion)
lean backwards with knes straight (extension) - no extension in facet disease.
Can do a modified Schobers Test - place index and middle fingers 5 centimeters apart and noting how close and far apart they move on the movements.
C-Spine
Lateral flexion: place your ear on your shoulder;
rotation: look over your shoulder;
flexion: put your chin on your chest;
extension: put your head back to look at the ceiling.
Thoracic
Fix pelvis and turn
- Special Tests
Straight leg raise - to look for sciatica
Sciatic nerve test - do SLR. When pain brought on, dorsiflex the foot = positive = sciatic!
Bowstring test - SLR. Then lower. Apply popliteal compression = symptoms.
Femoral nerve stretch test - lie prone, passively flex knee - severe = positive.
Tiptoe test - tests S1
Duck walk (on heels) - for L4 power
Neurological examination
References
http://www.osceskills.com/e-learning/subjects/spine-examination/
Thursday 22 September 2016
RSI
There are six separate phases of RSI.
1. Preoxygenation
Make sure you use your basic airway adjuncts as needed
Consider NODSAT
2. Preparation -
pre-assessment - use "LEMON" to see if you think the tube might be difficult
equipment - use a challenge and response checklist to make sure you have remembered everything, even capnography
position patient - find a pillow!
protect c-spine
3. Premedication
Fentanyl - onset 3 min, offset 20min
This can be useful in patients who have a head injury
4. Paralysis and Sedation
Paralysis -
Suxamethonium - depolarising. 1 - 1.5mg/kg bolus
10-20second onset with 3 - 5 minute offset
or Rocuronium - 1 - 1.5mg/kg
Hepatic and biliary excretion so longer offset time and longer onset time
Sedation
Propofol - 1.5 - 2.5mg/kg induction. Maintainence at 1-4 mg/kg/hr
15-20second onset, 5 - 10min offset
or Ketamine
We don't seem to use Thio or any of the others now.
5. Passage of the ETT - this is the very tricky bit that needs some theatre time!
6. Post intubation care
Complications of RSI
Failure to oxygenate - prevent by using checklist and DAS guidelines
Anaphylaxis - treat with anaphylaxis algorithm
Hypotension - turn down rate of sedation agent. Give small boluses of metaraminol or adrenaline IV to maintain BP.
Laryngospasm - oxygen, Larsens Notch
Apply PEEP
If this fails, paralyse and intubate (may be difficult)
Capnography
You need a good seal. If you have a poor trace this might be reflected in your capnography trace.
1. Preoxygenation
Make sure you use your basic airway adjuncts as needed
Consider NODSAT
2. Preparation -
pre-assessment - use "LEMON" to see if you think the tube might be difficult
equipment - use a challenge and response checklist to make sure you have remembered everything, even capnography
position patient - find a pillow!
protect c-spine
3. Premedication
Fentanyl - onset 3 min, offset 20min
This can be useful in patients who have a head injury
4. Paralysis and Sedation
Paralysis -
Suxamethonium - depolarising. 1 - 1.5mg/kg bolus
10-20second onset with 3 - 5 minute offset
or Rocuronium - 1 - 1.5mg/kg
Hepatic and biliary excretion so longer offset time and longer onset time
Sedation
Propofol - 1.5 - 2.5mg/kg induction. Maintainence at 1-4 mg/kg/hr
15-20second onset, 5 - 10min offset
or Ketamine
We don't seem to use Thio or any of the others now.
5. Passage of the ETT - this is the very tricky bit that needs some theatre time!
6. Post intubation care
Complications of RSI
Failure to oxygenate - prevent by using checklist and DAS guidelines
Anaphylaxis - treat with anaphylaxis algorithm
Hypotension - turn down rate of sedation agent. Give small boluses of metaraminol or adrenaline IV to maintain BP.
Laryngospasm - oxygen, Larsens Notch
Apply PEEP
If this fails, paralyse and intubate (may be difficult)
Capnography
You need a good seal. If you have a poor trace this might be reflected in your capnography trace.
Basic Airway Management
I hope we're pretty good at this!
Hands: head tilt chin lift or jaw thrust
Adjuncts: oropharyngeal airway -hard to hard preferred (middle of incisors to angle of jaw). Soft to soft (tragus to corner of mouth alternative)
nasopharyngeal 6mm women, 7mm men (not patient's little finger)
supraglottic airway eg. IGel
Tube: probably as an emergency RSI (see later)
Failed Intubation:
DAS Guidelines are really simple now and are easy to remember and follow.
Plan A: Intubate
Plan B: Supraglottic
Plan C: Facemask. Paralyse
Plan D: Front of neck surgical cric
Difficult BVM Assessment
M: Mask seal – for example a beard or blood
O: Obesity (BMI >30) and obstruction (snoring history)
A: Age >55
N: No teeth
S: Stiff lungs
Difficult Intubation Assessment
L: Look: a rapid ‘gut-feeling’ assessment
E: Evaluate the 3-3-2 rule
M: Mallampati score
O: Obesity/obstruction (stridor in particular is worrying)
N: Neck mobility
References and Further Links
http://learning.bmj.com/learning/modules/end/ELU.html?moduleId=10033823
https://www.das.uk.com/files/das2015intubation_guidelines.pdf
Hands: head tilt chin lift or jaw thrust
Adjuncts: oropharyngeal airway -hard to hard preferred (middle of incisors to angle of jaw). Soft to soft (tragus to corner of mouth alternative)
nasopharyngeal 6mm women, 7mm men (not patient's little finger)
supraglottic airway eg. IGel
Tube: probably as an emergency RSI (see later)
Failed Intubation:
DAS Guidelines are really simple now and are easy to remember and follow.
Plan A: Intubate
Plan B: Supraglottic
Plan C: Facemask. Paralyse
Plan D: Front of neck surgical cric
Difficult BVM Assessment
M: Mask seal – for example a beard or blood
O: Obesity (BMI >30) and obstruction (snoring history)
A: Age >55
N: No teeth
S: Stiff lungs
Difficult Intubation Assessment
L: Look: a rapid ‘gut-feeling’ assessment
E: Evaluate the 3-3-2 rule
M: Mallampati score
O: Obesity/obstruction (stridor in particular is worrying)
N: Neck mobility
References and Further Links
http://learning.bmj.com/learning/modules/end/ELU.html?moduleId=10033823
https://www.das.uk.com/files/das2015intubation_guidelines.pdf
Advanced Life Support
We all know how to manage cardiac arrest, as per ALS. There's always a few little things that I remember, and are good to remind ourselves of. There's also a few little things that we can do and think of as "extras".
Causes of Arrest
The 4Hs and 4Ts are commonly used, and this picture on the left (from Twitter, original source unknown) is a nice way of thinking about it.
Pyrexia must be prohibited post-cardiac arrest. It is common in the first 48 hours and the risk of a poor neurological outcome increases with each degree rise over 37oC. Maintain normothermia - 32 to 36 degrees.
If we have PEA, it is useful for us to think "Is it wide" or "is it narrow" to help us further hone our diagnostic reasoning.
Drugs
Post ROSC Care
A MAP of about 65-100 mmHg is a reasonable starting point in most –adjusted according to response.
"Special" Circumstances
Hypothermia: No adrenaline until >30,
double time in between 30 - 35,
normal once >35
Drugs are often ineffective and will undergo reduced metabolism.
In primary hypothermic cardiac arrest, death should not be confirmed until:
The patient has been re-warmed
Or
Other unsurvivable injuries have been identified
Or
Re-warming has failed despite all available measures
LA OD
Intralipid
1.5ml/kg bolus AND infusion 15ml/kg / hour
After 5 min 2 further boluses if not better
And double infusion to 30m/kg/hr
Resuscitate for one hour
Lidocaine toxicity
5 Light headedness, circumoral paraesthesia, slurred speech + tinnitus
10 Convulsions, LOC
15 Coma, myocardial depression
20 Resp arrest + arrhythmia
>25 Cardiac arrest
Pregnancy
Peri-mortem c-section
References and Links
http://rebelem.com/a-new-pulseless-electrical-activity-algorithm/
http://www.rcemlearning.co.uk/modules/an-unusual-cause-of-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/ooh-cardiac-arrest/
http://www.rcemlearning.co.uk/references/post-cardiac-arrest-care-of-the-rosc-patient/
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/management-of-post-arrest-patients-including-prognostication/
http://www.rcemlearning.co.uk/modules/a-systematic-review-of-therapeutic-hypothermia-for-non-shockable-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-hypothermic-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/modules/the-curious-incident-of-the-wolff-in-the-nighttime/
http://www.rcemlearning.co.uk/modules/the-resus-lottery/
http://www.rcemfoamed.co.uk/portfolio/saap-intra-aortic-adrenaline-in-cardiac-arrest/
Causes of Arrest
The 4Hs and 4Ts are commonly used, and this picture on the left (from Twitter, original source unknown) is a nice way of thinking about it.
Pyrexia must be prohibited post-cardiac arrest. It is common in the first 48 hours and the risk of a poor neurological outcome increases with each degree rise over 37oC. Maintain normothermia - 32 to 36 degrees.
If we have PEA, it is useful for us to think "Is it wide" or "is it narrow" to help us further hone our diagnostic reasoning.
Drugs
— Salim R. Rezaie (@srrezaie) September 29, 2015
Post ROSC Care
A MAP of about 65-100 mmHg is a reasonable starting point in most –adjusted according to response.
"Special" Circumstances
Hypothermia: No adrenaline until >30,
double time in between 30 - 35,
normal once >35
Drugs are often ineffective and will undergo reduced metabolism.
In primary hypothermic cardiac arrest, death should not be confirmed until:
The patient has been re-warmed
Or
Other unsurvivable injuries have been identified
Or
Re-warming has failed despite all available measures
LA OD
Intralipid
1.5ml/kg bolus AND infusion 15ml/kg / hour
After 5 min 2 further boluses if not better
And double infusion to 30m/kg/hr
Resuscitate for one hour
Lidocaine toxicity
5 Light headedness, circumoral paraesthesia, slurred speech + tinnitus
10 Convulsions, LOC
15 Coma, myocardial depression
20 Resp arrest + arrhythmia
>25 Cardiac arrest
Pregnancy
Peri-mortem c-section
http://rebelem.com/a-new-pulseless-electrical-activity-algorithm/
http://www.rcemlearning.co.uk/modules/an-unusual-cause-of-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/ooh-cardiac-arrest/
http://www.rcemlearning.co.uk/references/post-cardiac-arrest-care-of-the-rosc-patient/
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/management-of-post-arrest-patients-including-prognostication/
http://www.rcemlearning.co.uk/modules/a-systematic-review-of-therapeutic-hypothermia-for-non-shockable-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-hypothermic-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/modules/the-curious-incident-of-the-wolff-in-the-nighttime/
http://www.rcemlearning.co.uk/modules/the-resus-lottery/
http://www.rcemfoamed.co.uk/portfolio/saap-intra-aortic-adrenaline-in-cardiac-arrest/
Anaphylaxis
Anaphylaxis is not common, but as prompt treatment is so essential we need to know about it. It's similar in children (covered here) and adults.
Biphasic response occurs in 20% - much debate now about whether or not we need to observe people.
Causes
Antibiotics, especially penicillin
Aspirin
NSAIDs (the second most common cause of drug induced anaphylaxis)
Angiotensin Converting Enzyme Inhibitors
Treatment
Resus Council Algorithm
- Bue needle to inject adrenaline – orange is too short.
- IM injection in the anterolateral aspect of the thigh is best – it is absorbed quicker here than in the deltoid.
- No evidence to support use of H1 antihistamines in anaphylaxis (Sheikh et al 2007). Some evidence of improved skin signs e.g. itching for less severe reactions. Important to remember they can also cause drowsiness, confusion, fatigue and dizziness as side effects.
- H2-antihistamines = no evidence to support their routine use in anaphylaxis (Nurmatov et al 2014). May provide some relief for less emergent skin symptoms.
- Steroids (glucocorticoids) = no evidence to support their routine use in anaphylaxis (Choo et al 2012). The primary reason for administration has been to prevent biphasic reactions (see below), however a recent paper by Grunau et al (2015) found they were not associated with decreased relapses within 7 days.
Investigations
Tryptase sensitivity is low – 21%, especially to foods. It's not recommended in children.
Check tryptase as soon as resuscitation has started, 1-2 hours after symptoms, 24 hours later or in convalescence (some people have raised baseline tryptase levels).
"Special" Anaphylaxis
 Hereditary Angioedema
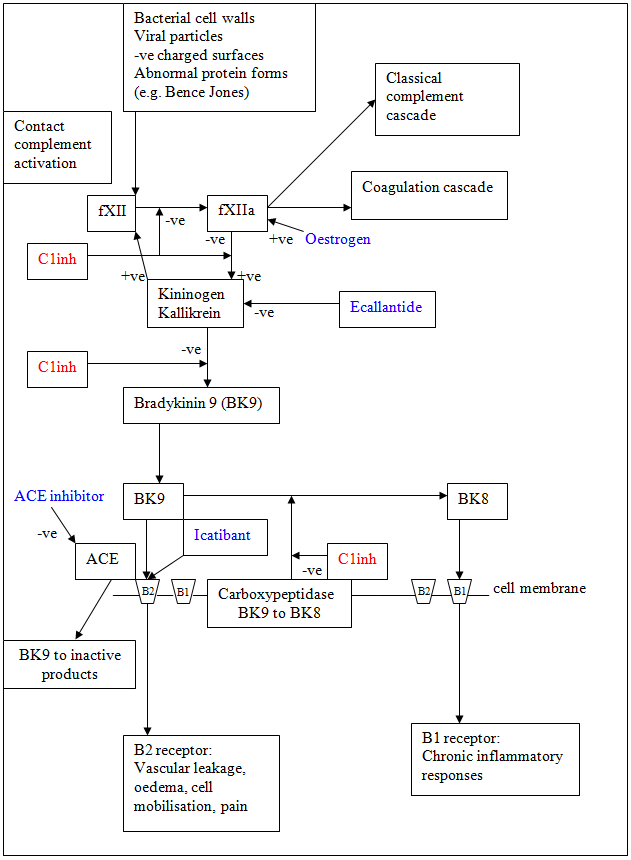
Hereditary AngioedemaOften doesn't respond to initial treatment. There's a good picture on RCEMLearning that shows how bradykinin is produced, both from ACE and oestrogen - and this can cause oedema.
Treat with concentrations of plasma and recombinant derived C1 inhibitor, or FFP if that isn't available.
Tranexamic acid may be helpful.
ACE Inhibitor
Excessive accumulation of bradykinin. Usually occurs soon after starting ACEi, but may be years later. Higher incidence amongst women, and African Americans.
It tends to be slowly evolving, with no urticarial or itching. Starts with focal, often asymmetric swelling.
Manage similar to C1 esterase inhibitor deficiency – give some FFP.
Kounis Syndrome
Anaphylaxis of the coronary arteries – maybe with or without existing coronary disease. There are lots of mast cells in the coronary arteries of people with coronary artery diseases. Coronary vasospasm is induced. There are no guidelines on how to treat it!
References and Further Reading
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/anaphylaxis/pre-test/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/references/anaphylaxis/
http://www.rcemlearning.co.uk/references/hereditary-angioedema/
http://calgaryguide.ucalgary.ca/type-i-hypersensitivity-pathogenesis-and-clinical-findings/
http://lifeinthefastlane.com/anaphylaxis-amplification/
http://thesgem.com/2013/12/sgem57-should-i-stay-or-should-i-go-biphasic-anaphylactic-response/
http://coreem.net/journal-reviews/biphasic-reactions-in-emergency-department-patients-with-allergic-reactions-or-anaphylaxis/
http://www.ncbi.nlm.nih.gov/pubmed/24239340
https://www.resus.org.uk/anaphylaxis/emergency-treatment-of-anaphylactic-reactions/
http://secure.rcem.ac.uk/code/document.asp?ID=5072
http://kcgs/Documents/CDUPruh013.pdf
http://kcgs/Documents/CDU002.pdf
emergencymedicinecases.com/anaphylaxis-anaphylactic-shock/
http://paediatricem.blogspot.co.uk/2013/07/anaphylaxis_29.html
Monday 15 August 2016
Vertigo
Vertigo is a very difficult topic. Although typically the diagnosis is split into central vs peripheral, it's probably better to think of it as
- investigate now
- investigate later
- No investigations needed.
Peripheral does not equal benign -> eg acoustic neuroma
Central does not equal life threatening -> migraine. Central rarely occurs in isolation, is less intense than peripheral, not possitional, hearing loss and tinnitus are rare and nystagmus is not inhibited by ocular fixation.It normally persists for more than 48 hours. Mild nausea and vomiting.
There are a few great flow charts, and lots of things to think about to work out what the cause is.
1. How long does it last for?
Seconds (psychogenic), Less than 1 min (BPPV), Minutes (Vascular/Ischaemic), Hours
(Meniere's or vestibular migraine), Hours to days (vestibular neuronitis, central causes, MS), Recurrent with headaches (Vestibular migraines).
2. Is it central or peripheral?
3. Dix - Hallpike to see if it's BPPV (peripheral cause)
Don't do it if there's any neck pathology that would make the procedure harmful - like arthritis. If patient dizzy on turning over in bed, BPPV is possible.
Patient in middle of bed. Looks towards one end of bed. Quickly lie flat.
Then over and up to the other side of the couch
Look for nystagmus
Nystagmus is diagnostic.
5. Treat the BPPV with Epley manueuvere:
Lie patient down
Head over couch
Look to side
Quickly turn head to other side - look for nystagmus. Stay there for 30 - 6o sec
Prepare to look at the floor - keep head still and roll onto side
Quickly look at floor
Stay for 30 - 60 seconds
Then sit up and put head down to keep looking at the floor
6. If it's central, HINTs
HI – Head impulse test: This test is a test of the patient vestibulo-occular reflex
Ask patient to look at a fixed target. Rapidly rotate head and look at eyes. A patient with an intact vestibulo-occular reflects will be able to maintain their gaze on the fixed target. The patient who has a defect with one of the vestibules will not be able to maintain gaze and as the head is rotated the eyes will rotate with the head away from the target, after a brief pause will then saccade back to the target. This can be subtle and some people have suggested that it can help
to use a phone with a slow motion app to capture the eye movements.
N - Nystagmus: Nystagmus mixed in peripheral, horizontal in central.
Peripheral vertigo decreases with fixation. Central vertigo persists with fixation.
Peripheral fatigues, central doesn't.
Horizontal, unidirectional never vertical in peripheral vertigo. Any direction for central vertigo.
In peripheral nystagmus resolves within 48 hours, and in central persists beyond 48 hours.
TS- Test of skew: Cerebellum and midbrain are required to allow the eyes to maintain fixed on their target during binocular vision. Cover each eye in turn and when an eye is uncovered looking for vertical deviation of the uncovered eye suggesting the presence of a central lesion.
7. Central Causes
Need ongoing referral and investigation. MRI in the first 48 hours misses 10 - 30% Posterior Circulation Strokes.
8. Treatment
Betahistine is for Meniere's disease only. Seak secondary care advice before starting.
9. Other Investigations
Arrhythmias are rarely the cause of dizziness, but it's worth having a look just incase.
ECG Abnormalities suggestive of arrhythmic syncope
Bifascicular block
Prolonged QRS
Mobitz 1
Brady <50bmp
Sinus pause >3sec
Pre-excited QRS
Long QT
RBBB with ST elevation (Brugada)
10. Look for red flag features
Headache 40% posterior circulation stroke
Gait ataxia May be only non‑vertiginous manifestation of cerebellar stroke
Hyperacute onset Suggests vascular origin
Vertigo and hearing loss AICA or urgent ENT problem
Prolonged symptoms (greater than 4 days) Floor of fourth ventricle problem
Symptoms on valsalva Perilymphatic fistula
References
https://vertigoed.wordpress.com/
http://www.londonscn.nhs.uk/wp-content/uploads/2016/04/neuro-adult-with-dizzy-spells-edu-videos-042016.pdf
http://www.rcemlearning.co.uk/modules/vertigo-will-it-make-your-head-spin/
- investigate now
- investigate later
- No investigations needed.
Peripheral does not equal benign -> eg acoustic neuroma
Central does not equal life threatening -> migraine. Central rarely occurs in isolation, is less intense than peripheral, not possitional, hearing loss and tinnitus are rare and nystagmus is not inhibited by ocular fixation.It normally persists for more than 48 hours. Mild nausea and vomiting.
There are a few great flow charts, and lots of things to think about to work out what the cause is.
1. How long does it last for?
Seconds (psychogenic), Less than 1 min (BPPV), Minutes (Vascular/Ischaemic), Hours
(Meniere's or vestibular migraine), Hours to days (vestibular neuronitis, central causes, MS), Recurrent with headaches (Vestibular migraines).
2. Is it central or peripheral?
3. Dix - Hallpike to see if it's BPPV (peripheral cause)
Don't do it if there's any neck pathology that would make the procedure harmful - like arthritis. If patient dizzy on turning over in bed, BPPV is possible.
Patient in middle of bed. Looks towards one end of bed. Quickly lie flat.
Then over and up to the other side of the couch
Look for nystagmus
Nystagmus is diagnostic.
5. Treat the BPPV with Epley manueuvere:
Lie patient down
Head over couch
Look to side
Quickly turn head to other side - look for nystagmus. Stay there for 30 - 6o sec
Prepare to look at the floor - keep head still and roll onto side
Quickly look at floor
Stay for 30 - 60 seconds
Then sit up and put head down to keep looking at the floor
6. If it's central, HINTs
HI – Head impulse test: This test is a test of the patient vestibulo-occular reflex
Ask patient to look at a fixed target. Rapidly rotate head and look at eyes. A patient with an intact vestibulo-occular reflects will be able to maintain their gaze on the fixed target. The patient who has a defect with one of the vestibules will not be able to maintain gaze and as the head is rotated the eyes will rotate with the head away from the target, after a brief pause will then saccade back to the target. This can be subtle and some people have suggested that it can help
to use a phone with a slow motion app to capture the eye movements.
N - Nystagmus: Nystagmus mixed in peripheral, horizontal in central.
Peripheral vertigo decreases with fixation. Central vertigo persists with fixation.
Peripheral fatigues, central doesn't.
Horizontal, unidirectional never vertical in peripheral vertigo. Any direction for central vertigo.
In peripheral nystagmus resolves within 48 hours, and in central persists beyond 48 hours.
TS- Test of skew: Cerebellum and midbrain are required to allow the eyes to maintain fixed on their target during binocular vision. Cover each eye in turn and when an eye is uncovered looking for vertical deviation of the uncovered eye suggesting the presence of a central lesion.
7. Central Causes
Need ongoing referral and investigation. MRI in the first 48 hours misses 10 - 30% Posterior Circulation Strokes.
8. Treatment
Betahistine is for Meniere's disease only. Seak secondary care advice before starting.
9. Other Investigations
Arrhythmias are rarely the cause of dizziness, but it's worth having a look just incase.
ECG Abnormalities suggestive of arrhythmic syncope
Bifascicular block
Prolonged QRS
Mobitz 1
Brady <50bmp
Sinus pause >3sec
Pre-excited QRS
Long QT
RBBB with ST elevation (Brugada)
10. Look for red flag features
Headache 40% posterior circulation stroke
Gait ataxia May be only non‑vertiginous manifestation of cerebellar stroke
Hyperacute onset Suggests vascular origin
Vertigo and hearing loss AICA or urgent ENT problem
Prolonged symptoms (greater than 4 days) Floor of fourth ventricle problem
Symptoms on valsalva Perilymphatic fistula
References
https://vertigoed.wordpress.com/
http://www.londonscn.nhs.uk/wp-content/uploads/2016/04/neuro-adult-with-dizzy-spells-edu-videos-042016.pdf
http://www.rcemlearning.co.uk/modules/vertigo-will-it-make-your-head-spin/
Sunday 14 August 2016
Sepsis
So Sepsis confuses me. There's loads of guidelines we're supposed to follow (some with out of date evidence) and it's not as simple as it could be. I've tried to simplify it... but might easily have misinterpreted something!
CEM and Surviving Sepsis Criteria define with SIRS
Need at least two of:
Temp > 38.3 Temp <36
WCC >12 or WCC <4
HR >90 RR >20
AMS BM >7.7
Patients with at least two SIRS criteria and suspected infective source should have the sepsis six delivered ASAP (within three hours of time of presentation according to surviving sepsis, within an hour if severe sepsis according to RCEM and most trusts). Surviving sepsis state within six hours of presentation we need vasopressors, re-assessment and re-check of the lactate.
Septic Shock – need vasopressors to keep MAP >65, lactate >2 despite fluid resuscitation. Sepsis 6 – 30mg/ kg for hypotension or lactate >4.
SOFA Scores
New studies have shown that SIRS is non specific and should no longer used for sepsis prognosis. They instead suggest a “SOFA (sepsis related organ failure assessment)” score where a changing score of > 2 = mortality of 10%.
The Qsofa is a quick bedside alternative, and >2 factors + suspected infection should make you think of sepsis:
"BAT" BP <100
AMS
Tachypnoea RR >22
This has not made its way into national guidelines yet.
RCEM Guidelines
Screen for sepsis using “SIRS criteria”
Sepsis risk stratify. Start sepsis six immediately if any one of:
• SBP <90mmHg or >40mmHg fall from baseline
• MAP <65mmHg
• Heart rate >130 per minute*
• New need for supplemental oxygen to maintain saturations >90% and bilateral infiltrates.
• Respiratory rate >25 per minute*
• AVPU = V, P or U*
• PaO2 / FiO2 ratio <300 (mmHg) or <39.9 (kPa)
• Lactate >2.0mmol/L
• Creatinine >176.8µmol/L
• INR >1.5
• aPTT >60s
• Platelet count <100 x109/L
• Bilirubin >34.2µmol
• Urine output <0.5mL/kg for two consecutive hours
Uncomplicated Sepsis: Decide whether to initiate sepsis six or not, >ST4 review within an hour, hourly obs, repeat lactate in two hours.
Red Flag Sepsis: HR > 130, AVPU less than A, RR >25
If blood results not confirmatory for severe sepsis, senior to review.
Red Flag or Severe: Severe sepsis is no longer in the Sepsis definitions but is in the RCEM guideline. Sepsis six ASAP, but within 60 minutes. >ST4 review. Obs 30minly. Repeat lactate.
Septic Shock: As above. Inform EM Consultant. Refer to outreach. Persisting hypotension requiring vasopressors to maintain MAP. Blood lactate >2mmol/L despite adequate volume resuscitation.
NICE Guidelines – July 2016
High risk of sepsis: in <1 year and >75 (or very frail). Immunosuppressed – by drugs or disease. Surgery in past six weeks. Breach of skin integrity. IV drug user. Indwelling lines or catheters. Pregnant or <6 weeks post partum.
Risk stratification for 12years and older – history. Respiratory (>25 or >40% FiO2 to keep sats >92% = high. Moderate = RR 21 – 24). BP (High = <90 or >40 below normal. Mod =91 – 100mmg Hg.). Circ (High = HR >130 bpm, anuric 18 hours, <0.5ml/hour if catheterised. Mod = HR 91 – 130 or new arrhythmia. Anuric 12 – 18 hours. 0.5 – 1ml / kg). Temp (Mod = temp <36). Skin (High = mottled or ashen, cyanosis, non blanching rash. Mod = Skin signs of infection).
There is a different stratification for children <5, and aged 5 – 11.
If >1 high risk criteria, senior clinical decision maker to review. Tests for glucose, lactate, cultures, FBC, CRP, U&E, creatinine, clotting. Antibiotics. Discuss with a Consultant. If septic shock, IV fluids stat, and refer to critical care. If lactate 2-4, give IV fluid bolus within an hour. Lactate <2, consider IV fluids. Monitor every 30minly. Consultant to r/v if failure to respond.
CEM Standards – severe sepsis and septic shock
Observe temp, PR, RR, BP, Mental status, BM on arrival.
Senior EM review within an hour
High flow O2 before leaving ED
Lactate, blood cultures
20mls/ kg fluid – 75% within an hour of arrival, 100% before leaving ED. Antibiotics – 50% within an hour, 100% before leaving ED.
Urine output measured before leaving the ED.
Trials
EGDT: Rivers. Found mortality benefit for EGDT.
ProCESS: Looked at protocol resus vs. usual car in septic shock. More ICU admissions in EGDT group. No difference otherwise.
ARISE: Australia. No advantage of EGDT.
PromMISe: UK based. No advantage over EGDT, which also increases costs.
Some theories: busted!
• Activated protein C - doesn't work
• Steroids - don't work, may be a small role only.
• Intensive insulin therapy - was based on harm from hyperglycaemia now used as moderate therapy only.
CRP
C reactive protein (CRP) is a protein produced by the liver in response to triggers from macrophages and adipose cells, which binds to the surface of dead or dying cells to activate the complement system.
CRP will rise within 2 hours of inflammation onset and peak at 48hrs. A normal level of CRP is not truly known.
References and Resources
http://www.rcem.ac.uk/Shop-Floor/Clinical%20Standards/Sepsis
http://www.heftemcast.co.uk/sepsis-in-the-ed/
http://www.heftemcast.co.uk/sepsis-smaccback/
http://www.frca.co.uk/article.aspx?articleid=100855
http://stemlynsblog.org/early-goal-directed-therapy-dead-st-emlyns/
http://www.survivingsepsis.org/SiteCollectionDocuments/SSC_Bundle.pdf http://stemlynsblog.org/the-promise-study-egdt-rip/
http://stemlynsblog.org/surviving-sepsis-update/
http://foam4gp.com/2015/07/23/foam4gp-map-my-esr-is-bigger-than-your-crp-or-do-we-care-not/
Sepsis = life threatening organ dysfunction due to dysregulated host response to infection. “SOFA” helps define and “prove” organ dysfunction.
CEM and Surviving Sepsis Criteria define with SIRS
Need at least two of:
Temp > 38.3 Temp <36
WCC >12 or WCC <4
HR >90 RR >20
AMS BM >7.7
Patients with at least two SIRS criteria and suspected infective source should have the sepsis six delivered ASAP (within three hours of time of presentation according to surviving sepsis, within an hour if severe sepsis according to RCEM and most trusts). Surviving sepsis state within six hours of presentation we need vasopressors, re-assessment and re-check of the lactate.
Septic Shock – need vasopressors to keep MAP >65, lactate >2 despite fluid resuscitation. Sepsis 6 – 30mg/ kg for hypotension or lactate >4.
SOFA Scores
New studies have shown that SIRS is non specific and should no longer used for sepsis prognosis. They instead suggest a “SOFA (sepsis related organ failure assessment)” score where a changing score of > 2 = mortality of 10%.
The Qsofa is a quick bedside alternative, and >2 factors + suspected infection should make you think of sepsis:
"BAT" BP <100
AMS
Tachypnoea RR >22
This has not made its way into national guidelines yet.
RCEM Guidelines
Screen for sepsis using “SIRS criteria”
Sepsis risk stratify. Start sepsis six immediately if any one of:
• SBP <90mmHg or >40mmHg fall from baseline
• MAP <65mmHg
• Heart rate >130 per minute*
• New need for supplemental oxygen to maintain saturations >90% and bilateral infiltrates.
• Respiratory rate >25 per minute*
• AVPU = V, P or U*
• PaO2 / FiO2 ratio <300 (mmHg) or <39.9 (kPa)
• Lactate >2.0mmol/L
• Creatinine >176.8µmol/L
• INR >1.5
• aPTT >60s
• Platelet count <100 x109/L
• Bilirubin >34.2µmol
• Urine output <0.5mL/kg for two consecutive hours
Uncomplicated Sepsis: Decide whether to initiate sepsis six or not, >ST4 review within an hour, hourly obs, repeat lactate in two hours.
Red Flag Sepsis: HR > 130, AVPU less than A, RR >25
If blood results not confirmatory for severe sepsis, senior to review.
Red Flag or Severe: Severe sepsis is no longer in the Sepsis definitions but is in the RCEM guideline. Sepsis six ASAP, but within 60 minutes. >ST4 review. Obs 30minly. Repeat lactate.
Septic Shock: As above. Inform EM Consultant. Refer to outreach. Persisting hypotension requiring vasopressors to maintain MAP. Blood lactate >2mmol/L despite adequate volume resuscitation.
NICE Guidelines – July 2016
High risk of sepsis: in <1 year and >75 (or very frail). Immunosuppressed – by drugs or disease. Surgery in past six weeks. Breach of skin integrity. IV drug user. Indwelling lines or catheters. Pregnant or <6 weeks post partum.
Risk stratification for 12years and older – history. Respiratory (>25 or >40% FiO2 to keep sats >92% = high. Moderate = RR 21 – 24). BP (High = <90 or >40 below normal. Mod =91 – 100mmg Hg.). Circ (High = HR >130 bpm, anuric 18 hours, <0.5ml/hour if catheterised. Mod = HR 91 – 130 or new arrhythmia. Anuric 12 – 18 hours. 0.5 – 1ml / kg). Temp (Mod = temp <36). Skin (High = mottled or ashen, cyanosis, non blanching rash. Mod = Skin signs of infection).
There is a different stratification for children <5, and aged 5 – 11.
If >1 high risk criteria, senior clinical decision maker to review. Tests for glucose, lactate, cultures, FBC, CRP, U&E, creatinine, clotting. Antibiotics. Discuss with a Consultant. If septic shock, IV fluids stat, and refer to critical care. If lactate 2-4, give IV fluid bolus within an hour. Lactate <2, consider IV fluids. Monitor every 30minly. Consultant to r/v if failure to respond.
CEM Standards – severe sepsis and septic shock
Observe temp, PR, RR, BP, Mental status, BM on arrival.
Senior EM review within an hour
High flow O2 before leaving ED
Lactate, blood cultures
20mls/ kg fluid – 75% within an hour of arrival, 100% before leaving ED. Antibiotics – 50% within an hour, 100% before leaving ED.
Urine output measured before leaving the ED.
Trials
EGDT: Rivers. Found mortality benefit for EGDT.
ProCESS: Looked at protocol resus vs. usual car in septic shock. More ICU admissions in EGDT group. No difference otherwise.
ARISE: Australia. No advantage of EGDT.
PromMISe: UK based. No advantage over EGDT, which also increases costs.
Some theories: busted!
• Activated protein C - doesn't work
• Steroids - don't work, may be a small role only.
• Intensive insulin therapy - was based on harm from hyperglycaemia now used as moderate therapy only.
CRP
C reactive protein (CRP) is a protein produced by the liver in response to triggers from macrophages and adipose cells, which binds to the surface of dead or dying cells to activate the complement system.
CRP will rise within 2 hours of inflammation onset and peak at 48hrs. A normal level of CRP is not truly known.
References and Resources
http://www.rcem.ac.uk/Shop-Floor/Clinical%20Standards/Sepsis
http://www.heftemcast.co.uk/sepsis-in-the-ed/
http://www.heftemcast.co.uk/sepsis-smaccback/
http://www.frca.co.uk/article.aspx?articleid=100855
http://stemlynsblog.org/early-goal-directed-therapy-dead-st-emlyns/
http://www.survivingsepsis.org/SiteCollectionDocuments/SSC_Bundle.pdf http://stemlynsblog.org/the-promise-study-egdt-rip/
http://stemlynsblog.org/surviving-sepsis-update/
http://foam4gp.com/2015/07/23/foam4gp-map-my-esr-is-bigger-than-your-crp-or-do-we-care-not/
Thursday 2 June 2016
Iron Overdose
Iron overdose is common, but it is infrequent that it causes severe problems. I have seen it frequently in children, who take their parents well woman tablets, or similar.
Background
When thinking about iron, the first thing that must be done is to convert the amount of iron taken, to the amount of elemental iron ingested. This varies considerably between different types of iron tablets, depending on the type of ferrous or ferric salt:
ferrous sulfate (dried) — divide dose by 3.3
ferrous sulfate (heptahydrate) — divide dose by 5
ferrous gluconate — divide dose by 9
ferrous fumarate — divide dose by 3
ferric chloride — divide dose by 3.5
ferrous chloride — divide dose by 4
You can then risk stratify, by the amount of elemental iron they have ingested:
<20mg/kg –– asymptomatic
20-60mg/kg –– GI symptoms only
60-120mg/kg –– potential for systemic toxicity
>120mg/kg –– potentially lethal
Peak serum iron levels occur 4-6 hours following iron ingestion, then levels fall due to intracellular shift. Levels do not clearly correlate with clinical toxicity, but > 90 micromol/L (500 mcg/dL) is generally considered predictive of systemic toxicity (equivalent to >60mg/kg)
Pathophysiology
Local Effects - corrosive injury to the GI mucosa (vomiting, diarrhoea, haematemeis, melaena) . Can lead to gastric strictures.
Systemic Effects - cellular toxin, targeting the cardiovascular syndrome. Severe lactic acidosis from hypoperfusion due to volume loss, vasodilation and negative inotropic effects.
Clinical Symptoms

Investigations
Blood gas - can look like DKA. Anion gap metabolic acidosis.
BMs - can be hyperglycaemic
AXR
LFTs, Coags — hepatic failure
U&E — renal failure
Iron levels
Management
**Not adsorbed by activated charcoal**
Whole bowel irrigation for ingestion >60mg/kg
Surgical or endoscopy removal if >120mg/kg or WBI not feasible
Desferroxamine Chelation:
level >90 micromol/L at 4-6 hours post-ingestion
evidence of systemic toxicity
shock
metabolic acidosis
altered mental status
Chelates free irons that can be renally excreted. Ferrioxamine is then excreted unchanged in the urine which classically, not reliably, turns a vin rose colour.
15 mg/kg/h, reduced if hypotension occurs, may be titrated up to 40mg/kg/h in severe toxicity
cardiac monitoring is mandatory. Can cause hypersensitivity, ARDS, toxic retinopathy or yersinia sepsis. Can be stopped when the patient is stable and serum iron is <60micromol/L - usually 56 hours.
References
http://learning.bmj.com/learning/modules/elucidat/57067260702df.html?moduleId=10055999&status=LIVE&action=start&_flowId=ELU&sessionTimeoutInMin=90&locale=en_GB&shouldStartAtQuestionSection=false
https://www.aliem.com/2014/management-iron-toxicity/
http://lifeinthefastlane.com/ccc/iron-overdose/
http://lifeinthefastlane.com/toxicology-conundrum-034/
https://wikem.org/wiki/Iron_toxicity
http://lifeinthefastlane.com/tox-library/antidote/desferrioxamine/
http://www.foamem.com/2014/08/06/management-of-iron-toxicity/
http://adc.bmj.com/content/87/5/400.full
http://lifeinthefastlane.com/cicm-saq-2009-2-q18/
Background
When thinking about iron, the first thing that must be done is to convert the amount of iron taken, to the amount of elemental iron ingested. This varies considerably between different types of iron tablets, depending on the type of ferrous or ferric salt:
ferrous sulfate (dried) — divide dose by 3.3
ferrous sulfate (heptahydrate) — divide dose by 5
ferrous gluconate — divide dose by 9
ferrous fumarate — divide dose by 3
ferric chloride — divide dose by 3.5
ferrous chloride — divide dose by 4
You can then risk stratify, by the amount of elemental iron they have ingested:
<20mg/kg –– asymptomatic
20-60mg/kg –– GI symptoms only
60-120mg/kg –– potential for systemic toxicity
>120mg/kg –– potentially lethal
Peak serum iron levels occur 4-6 hours following iron ingestion, then levels fall due to intracellular shift. Levels do not clearly correlate with clinical toxicity, but > 90 micromol/L (500 mcg/dL) is generally considered predictive of systemic toxicity (equivalent to >60mg/kg)
Local Effects - corrosive injury to the GI mucosa (vomiting, diarrhoea, haematemeis, melaena) . Can lead to gastric strictures.
Systemic Effects - cellular toxin, targeting the cardiovascular syndrome. Severe lactic acidosis from hypoperfusion due to volume loss, vasodilation and negative inotropic effects.
Clinical Symptoms

Investigations
Blood gas - can look like DKA. Anion gap metabolic acidosis.
BMs - can be hyperglycaemic
AXR
LFTs, Coags — hepatic failure
U&E — renal failure
Iron levels
Management
**Not adsorbed by activated charcoal**
Whole bowel irrigation for ingestion >60mg/kg
Surgical or endoscopy removal if >120mg/kg or WBI not feasible
Desferroxamine Chelation:
level >90 micromol/L at 4-6 hours post-ingestion
evidence of systemic toxicity
shock
metabolic acidosis
altered mental status
Chelates free irons that can be renally excreted. Ferrioxamine is then excreted unchanged in the urine which classically, not reliably, turns a vin rose colour.
15 mg/kg/h, reduced if hypotension occurs, may be titrated up to 40mg/kg/h in severe toxicity
cardiac monitoring is mandatory. Can cause hypersensitivity, ARDS, toxic retinopathy or yersinia sepsis. Can be stopped when the patient is stable and serum iron is <60micromol/L - usually 56 hours.
References
http://learning.bmj.com/learning/modules/elucidat/57067260702df.html?moduleId=10055999&status=LIVE&action=start&_flowId=ELU&sessionTimeoutInMin=90&locale=en_GB&shouldStartAtQuestionSection=false
https://www.aliem.com/2014/management-iron-toxicity/
http://lifeinthefastlane.com/ccc/iron-overdose/
http://lifeinthefastlane.com/toxicology-conundrum-034/
https://wikem.org/wiki/Iron_toxicity
http://lifeinthefastlane.com/tox-library/antidote/desferrioxamine/
http://www.foamem.com/2014/08/06/management-of-iron-toxicity/
http://adc.bmj.com/content/87/5/400.full
http://lifeinthefastlane.com/cicm-saq-2009-2-q18/
Monday 2 May 2016
Cough
Cough seems a strange thing to have on the syllabus, but we do see lots of patients presenting with cough. They often want antibiotics...and these aren't often the answer. The references at the bottom of the page have got some excellent management guidelines.
Acute Cough
Viral Cough - self limiting. No anti-tussive therapy needed. Efficacy of OTC medications is not compelling. Home based remedies like honey and lemon or honey and coffee.
Chronic Cough
Lasts >8 weeks. Mostly women, with an average age of 55. Can treat empirically before investigations.
Differentials
Pertussis
Tuberculosis
Pulmonary fibrosis - get honeycomb on the CT. Make sure you treat any concurrent reflux,
Reflux - if asymptomatic don't treat. Otherwise, PPI BD + ranitidine. Next step pro-kinetics like metoclopramide.
Drug Differentials
Latanoprost - augments cough-reflex sensitivity
ACE inhibitors - may take up to several months to stop. ACE inhibitors upregulate the cough reflex
Nitrofurantoin
Bleomycin, methotrexate and amiodarone may cause pulmonary fibrosis
Investigations
CXR
- if >40 and has ever smoked and has cough, fatigue, SOB, chest pain, weight or appetetite loss.
- if >40 and persistent or recurrent chest infection, clubbing, specific lymphadenopathy, chest signs consistent with lung cancer, thrombocytosis.
Spirometry
Consider checking for sleep apnoea - CPAP may help
Treatment
Treat cause - first generation antihistamines can help.
If cold related consider brompheniramine and SR pseudoephedrine. Naproxen can also help.
References
http://www.rcemlearning.co.uk/modules/a-constant-cough/
http://www.rcemlearning.co.uk/modules/bloody-cough/
http://www.rcemlearning.co.uk/exams/unusual-cough/
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1692
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1388
http://journal.publications.chestnet.org/data/Journals/CHEST/934853/51496.pdf
http://rebelem.com/long-cough-respiratory-illness-last/
https://www.brit-thoracic.org.uk/document-library/clinical-information/cough/cough-guidelines/recommendations-for-the-management-of-cough-in-adults/
https://www.brit-thoracic.org.uk/document-library/clinical-information/cough/cough-guidelines/recommendations-for-the-management-of-cough-in-children/
http://journal.publications.chestnet.org/data/Journals/CHEST/22039/1S.pdf
Acute Cough
Viral Cough - self limiting. No anti-tussive therapy needed. Efficacy of OTC medications is not compelling. Home based remedies like honey and lemon or honey and coffee.
Chronic Cough
Lasts >8 weeks. Mostly women, with an average age of 55. Can treat empirically before investigations.
Differentials
Pertussis
Tuberculosis
Pulmonary fibrosis - get honeycomb on the CT. Make sure you treat any concurrent reflux,
Reflux - if asymptomatic don't treat. Otherwise, PPI BD + ranitidine. Next step pro-kinetics like metoclopramide.
Drug Differentials
Latanoprost - augments cough-reflex sensitivity
ACE inhibitors - may take up to several months to stop. ACE inhibitors upregulate the cough reflex
Nitrofurantoin
Bleomycin, methotrexate and amiodarone may cause pulmonary fibrosis
Investigations
CXR
- if >40 and has ever smoked and has cough, fatigue, SOB, chest pain, weight or appetetite loss.
- if >40 and persistent or recurrent chest infection, clubbing, specific lymphadenopathy, chest signs consistent with lung cancer, thrombocytosis.
Spirometry
Consider checking for sleep apnoea - CPAP may help
Treatment
Treat cause - first generation antihistamines can help.
If cold related consider brompheniramine and SR pseudoephedrine. Naproxen can also help.
References
http://www.rcemlearning.co.uk/modules/a-constant-cough/
http://www.rcemlearning.co.uk/modules/bloody-cough/
http://www.rcemlearning.co.uk/exams/unusual-cough/
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1692
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1388
http://journal.publications.chestnet.org/data/Journals/CHEST/934853/51496.pdf
http://rebelem.com/long-cough-respiratory-illness-last/
https://www.brit-thoracic.org.uk/document-library/clinical-information/cough/cough-guidelines/recommendations-for-the-management-of-cough-in-adults/
https://www.brit-thoracic.org.uk/document-library/clinical-information/cough/cough-guidelines/recommendations-for-the-management-of-cough-in-children/
http://journal.publications.chestnet.org/data/Journals/CHEST/22039/1S.pdf
Friday 29 April 2016
CVP
The CVP
This is the pressure recorded from the right atrium or superior vena cava
It is representative of the filling pressure of the right side of the heart
Normal is 8- 12 mmHg in a spontaneously breathing non-ventilated patient
recorded at the end of expiration
It is made up of many different waves:
a = atrial contraction (dominant in pulmonary HTN, TS, PS)
c = closing and bulging of the tricuspid valve (cannon in heart block)
x = atrial relaxation (absent in AF, exaggerated in tamponade)
v = passive filling of atrium (dominant in TR)
y = opening of the tricuspid valve (sharp in severe TR, constrictive pericarditis. Slow in TR)
Raised CVP
Fluid overload (although there is a poor relationship)
High PEEP settings (PEEP of 10cm H20 = CVP increase 3cm H20)
Right ventricular failure
Tricuspid stenosis or regurgitation
Pericardial effusion or constrictive pericarditis
Superior vena caval obstruction
References
http://lifeinthefastlane.com/ccc/cvp-measurement/
Oxford Handbook of Critical Care
This is the pressure recorded from the right atrium or superior vena cava
It is representative of the filling pressure of the right side of the heart
Normal is 8- 12 mmHg in a spontaneously breathing non-ventilated patient
recorded at the end of expiration
It is made up of many different waves:
a = atrial contraction (dominant in pulmonary HTN, TS, PS)
c = closing and bulging of the tricuspid valve (cannon in heart block)
x = atrial relaxation (absent in AF, exaggerated in tamponade)
v = passive filling of atrium (dominant in TR)
y = opening of the tricuspid valve (sharp in severe TR, constrictive pericarditis. Slow in TR)
Raised CVP
Fluid overload (although there is a poor relationship)
High PEEP settings (PEEP of 10cm H20 = CVP increase 3cm H20)
Right ventricular failure
Tricuspid stenosis or regurgitation
Pericardial effusion or constrictive pericarditis
Superior vena caval obstruction
References
http://lifeinthefastlane.com/ccc/cvp-measurement/
Oxford Handbook of Critical Care
Tuesday 29 March 2016
Cyanosis
This seems like a random curriculum item to me. A quick trawl through the Oxford Handbook of EM suggests I need to think about:
Anaphylaxis
Asthma
COPD
Aspiration
Pulmonary Embolism
Seizure
Toxicology - opioid poisoning, paraquat lung, petrol and paraffin poisoning, anthrax
Respiratory distress - chest wall injury, pneumothorax
Uncommon in cyanide poisoning
LITFL splits it further
Central Causes - low sats, metHb, altitude
Peripheral Causes - cold, reduced cardiac output including congenital heart disease.
References
http://www.rcemlearning.co.uk/exams/he-looks-a-bit-blue-doctor/
http://www.rcemlearning.co.uk/modules/papa-smurf-has-a-seizure/
http://lifeinthefastlane.com/resources/cyanosis-ddx/
Oxygen Therapy
Administering extra oxygen is easy, but there are some more things we could and should think about. Once 30% or more of the blood in the pulmonary circulation passes through an area of low V/Q, the hypoxia cannot be corrected by simply increasing the oxygen content of the inspired gas.
Hypoxic Drive
Oxygen induced hypercapnea is likely to include:
- Worsened ventilation-perfusion mismatch (due to pulmonary vasoconstriction)
- Decreased binding affinity of haemoglobin for carbon dioxide
- Reduced minute ventilation.
So giving extra oxygen is unlikely to be a problem but we need to be aware of it, and monitor it.
Alveolar Gas Equation
PAO2 = 95 x FIO2(%) – 1.25 x PaCO2
Under normal circumstances the difference between this and the arterial O2 tension (PaO2) measured by the ABG machine is 2-4 kPa. This difference is known as the A-a gradient. Its calculation can help to distinguish between types of hypoxia.
References
http://learning.bmj.com/learning/module-intro/oxygen-therapy.html?moduleId=10053774&searchTerm=%E2%80%9Coxygen%E2%80%9D&page=1&locale=en_GB
http://www.rcemlearning.co.uk/modules/oxygen-in-human-physiology/
http://www.rcemfoamed.co.uk/portfolio/hypoxic-drive-fact-or-fiction/
http://emcrit.org/wp-content/uploads/2015/06/nejmoa1503326.pdf
http://www.annemergmed.com/article/S0196-0644(15)01500-0/abstract
Saturday 19 March 2016
Hyperkalaemia
Hyperkalaemia is a medical emergency that we should know how to manage. Following a guideline is easy - but sometimes we need to know more than just how to follow the guideline! So..if you have a high potassium consider:
1. Is it really hyperkalaemia?
- Prolonged TK time
- Haemolysis
- Acidosis causing transcellular shift
- The ABG analyser result does correlate well with a true result
2. Stop all likely causes
- Treat pre-renal (and renal) failure
- Stop drugs (amiloride, spironolactone, ACE inhibitors, NSAIDs)
3. Do an ECG
The changes don't appear at a set potassium level, but it does show the cardiac toxicity.
- Symmetrical T wave peaking - T wave looks uncomfortable to sit on
- PR interval prolongation
- Reduced P wave amplitude
- QRS complex widening
- sine wave formation
- Fine ventricular fibrillation and asystole
- Progressive bradycardia.
4. If ECG changes present, protect the heart - give some calcium.
Calcium Chloride - more toxic if extravasated
Calcium chloride contains about three times as much calcium as calcium gluconate (0.68 mmol/ml versus 0.22 mmol/ml) and has a greater bioavailability than gluconate. If you use calcium gluconate, you are more likely to need to give repeated doses.
Give slowly over 20min + 10ml glucose 5% if on digoxin, as rapid calcium administration may precipitate myocardial digoxin toxicity.
5. Shift Potassium into the cells
- Insulin-Glucose IV infusion
- Nebulised sabutamol
6. Remove potasium from the body
- Consider calcium resonium which takes >2 hours to work.
- Sodium bicarbonate may precipitate pulmonary oedema due to its sodium load, or tetany, and is not very effective. You cannot give calcium salts and sodium bicarbonate via the same intravenous line because this causes precipitation of calcium carbonate. May be more useful in acidotic patients.
- Furosemide can help if you have good urine output.
7. Monitor
8. Look for signs and symptoms
Muscle weakness and paraesthesia may occur in patients with severe hyperkalaemia and may progress to flaccid paralysis. The respiratory muscles are usually spared. Muscle weakness normally starts in the lower limbs and progresses to the trunk and upper limbs, and is more common when serum potassium is more than 8.0 mmol/l
Generalised twitching
Confusion
Pericardial friction rub
Urinary retention
9. Understand normal
How does the body handle the overall balance of potassium?
A normal Western diet contains about 100 mmol of potassium per day. Most potassium is renally excreted.
10. Recheck and Review
Recheck potassium level after 4 hours and as indicated according to the levels obtained.
References
http://learning.bmj.com/learning/module-intro/hyperkalaemia-diagnosis-management.html?moduleId=6055258&searchTerm=%E2%80%9Chyperkalaemia%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/hyperkalaemia.html?moduleId=10047565&searchTerm=%E2%80%9Chyperkalaemia%E2%80%9D&page=1&locale=en_GB
http://www.aliem.com/2013/mythbuster-calcium-gluconate-raises-serum-calcium-as-calcium-chloride/
http://first10em.com/2016/01/21/hyperkalemia/
http://www.rcemfoamed.co.uk/portfolio/hyperkalaemia/
1. Is it really hyperkalaemia?
- Prolonged TK time
- Haemolysis
- Acidosis causing transcellular shift
- The ABG analyser result does correlate well with a true result
2. Stop all likely causes
- Treat pre-renal (and renal) failure
- Stop drugs (amiloride, spironolactone, ACE inhibitors, NSAIDs)
3. Do an ECG
The changes don't appear at a set potassium level, but it does show the cardiac toxicity.
- Symmetrical T wave peaking - T wave looks uncomfortable to sit on
- PR interval prolongation
- Reduced P wave amplitude
- QRS complex widening
- sine wave formation
- Fine ventricular fibrillation and asystole
- Progressive bradycardia.
4. If ECG changes present, protect the heart - give some calcium.
Calcium Chloride - more toxic if extravasated
Calcium chloride contains about three times as much calcium as calcium gluconate (0.68 mmol/ml versus 0.22 mmol/ml) and has a greater bioavailability than gluconate. If you use calcium gluconate, you are more likely to need to give repeated doses.
Give slowly over 20min + 10ml glucose 5% if on digoxin, as rapid calcium administration may precipitate myocardial digoxin toxicity.
5. Shift Potassium into the cells
- Insulin-Glucose IV infusion
- Nebulised sabutamol
6. Remove potasium from the body
- Consider calcium resonium which takes >2 hours to work.
- Sodium bicarbonate may precipitate pulmonary oedema due to its sodium load, or tetany, and is not very effective. You cannot give calcium salts and sodium bicarbonate via the same intravenous line because this causes precipitation of calcium carbonate. May be more useful in acidotic patients.
- Furosemide can help if you have good urine output.
7. Monitor
8. Look for signs and symptoms
Muscle weakness and paraesthesia may occur in patients with severe hyperkalaemia and may progress to flaccid paralysis. The respiratory muscles are usually spared. Muscle weakness normally starts in the lower limbs and progresses to the trunk and upper limbs, and is more common when serum potassium is more than 8.0 mmol/l
Generalised twitching
Confusion
Pericardial friction rub
Urinary retention
9. Understand normal
How does the body handle the overall balance of potassium?
A normal Western diet contains about 100 mmol of potassium per day. Most potassium is renally excreted.
10. Recheck and Review
Recheck potassium level after 4 hours and as indicated according to the levels obtained.
References
http://learning.bmj.com/learning/module-intro/hyperkalaemia-diagnosis-management.html?moduleId=6055258&searchTerm=%E2%80%9Chyperkalaemia%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/hyperkalaemia.html?moduleId=10047565&searchTerm=%E2%80%9Chyperkalaemia%E2%80%9D&page=1&locale=en_GB
http://www.aliem.com/2013/mythbuster-calcium-gluconate-raises-serum-calcium-as-calcium-chloride/
http://first10em.com/2016/01/21/hyperkalemia/
http://www.rcemfoamed.co.uk/portfolio/hyperkalaemia/
Sunday 7 February 2016
Hyperventilation
The term "hyperventilation" is one I am not particularly fond of. I think there are three separate causes of hyperventilation:
- Pathological - eg PE, pneumonia, pain
- Iatrogenic - "overbagging"
- Panic / anxiety/ hysteria
The third is the cause of hyperventilation we are now going to focus on. It seems to me to be an exaggeration of a normal physiological response - a form of control system dysfunction. The respiratory distress is driven by the brain.
The DSM-IV criteria for a panic attack is quite specific. They define it as a period of intense fear or discomfort developing abruptly, and peaking within ten minutes + 4 of:
a. Chest pain/ discomfort, b. Chills or hot flushes, c. Derealisation or depersonalisation, d. Fear of loosing control, e. Feeling dizzy, f. Feeling of choking, g. Nausea, h. Palpitations, i. Paraesthesias. j. SOB, k. Impending doom, l, Sweating, m. Trembling
Carpopedal Spasm
- Rapid breathing results in excess excretion of carbon dioxide in the lungs
- This reduces the concentration of CO2 in the blood
- The blood pH becomes alkali
- This causes increased binding of calcium ions to proteins in the blood
- The reduced level of calcium causes "carpopedal spasm"
- This could also lead to tetany
Investigation
The lactate can be high - is not helpful
ABG would show a normal PO2 and a marked respiratory alkalosis. The Ca may be low.
Treatment
Control the breathing. This is really difficult to do, and very frustrating! Telling them to control their breathing or calm down is likely to make matters worse, not better.
- Give them a cold drink
- Ask them to read a sentence out loud
- Paper bags are NOT recommended - lots of patients ended up getting a paper bag for asthma
- Long term - CBT may be needed
References
Wednesday 27 January 2016
Methaemoglobin
Pathogenesis
- Oxidisation of the haem of haemoglobin by free radicals or things like hydrogen peroxide and nitric oxide.
- Shifts O2 dissociation curve to the left.
Causes
- Hereditary / Congenital: Hb and NADH-MetHb reductase deficiency
- Acquired:
* Medications eg. Amyl nitrite, Benzocaine, Dapsone, Lidocaine, Nitroglycerin, Nitroprusside, Phenacetin, Phenazopyridine, Prilocaine, Quinones, Sulfonamides (eg. sulfamethoxazole). Chloroquine.
* Chemical agents eg. Aniline dye derivatives (shoe dyes, inks) Butyl nitrite, Chlorobenzene, Nitrate-containing foods, Isobutyl nitrite, Naphthalene, Nitrophenol, Nitrous gases, Silver nitrate, and Trinitrotoluene. Sodium nitrite - used in food preservation.
Signs & Symptoms
- chocolate brown discoloration of the blood.
- SaO2 readings go crazy
0-10% - Features unlikely
10-30%- Mild effects
Blue-grey ‘apparent’ central cyanosis, fatigue, dizziness, headaches
30-50% - Moderate effects – weakness, tachypnoea, tachycardia
50-70% - Severe effects
stupor, coma, convulsions, respiratory depression, cardiac arrhythmias, acidosis
> 70% - Potentially fatal
Treatment
<20% - nothing
20 - 30% - oxygen therapy
>30% - methylene blue
1-2 mg/kg IV over 5 minutes - 1% (10mg/ml solution)
repeat up to 7 mg/kg
SpO2 normally dives as you give the methylene blue.
Recheck levels after an hour
Interesting Note
Hydrogen sulfide poisoning is similar to cyanide poisoning and can be treated by inducing metHb.
References
http://stemlynsblog.org/feeling-blue-at-st-emlyns/
http://www.rcemlearning.co.uk/modules/papa-smurf-has-a-seizure/
http://emergencymedicineireland.com/2011/07/why-methaemoglobinaemia-is-a-good-thing/
http://emergencymedicineireland.com/2011/07/why-methaemoglobinaemia-is-a-bad-thing/
- Oxidisation of the haem of haemoglobin by free radicals or things like hydrogen peroxide and nitric oxide.
- Shifts O2 dissociation curve to the left.
Causes
- Hereditary / Congenital: Hb and NADH-MetHb reductase deficiency
- Acquired:
* Medications eg. Amyl nitrite, Benzocaine, Dapsone, Lidocaine, Nitroglycerin, Nitroprusside, Phenacetin, Phenazopyridine, Prilocaine, Quinones, Sulfonamides (eg. sulfamethoxazole). Chloroquine.
* Chemical agents eg. Aniline dye derivatives (shoe dyes, inks) Butyl nitrite, Chlorobenzene, Nitrate-containing foods, Isobutyl nitrite, Naphthalene, Nitrophenol, Nitrous gases, Silver nitrate, and Trinitrotoluene. Sodium nitrite - used in food preservation.
Signs & Symptoms
- chocolate brown discoloration of the blood.
- SaO2 readings go crazy
0-10% - Features unlikely
10-30%- Mild effects
Blue-grey ‘apparent’ central cyanosis, fatigue, dizziness, headaches
30-50% - Moderate effects – weakness, tachypnoea, tachycardia
50-70% - Severe effects
stupor, coma, convulsions, respiratory depression, cardiac arrhythmias, acidosis
> 70% - Potentially fatal
Treatment
<20% - nothing
20 - 30% - oxygen therapy
>30% - methylene blue
1-2 mg/kg IV over 5 minutes - 1% (10mg/ml solution)
repeat up to 7 mg/kg
SpO2 normally dives as you give the methylene blue.
Recheck levels after an hour
Interesting Note
Hydrogen sulfide poisoning is similar to cyanide poisoning and can be treated by inducing metHb.
References
http://stemlynsblog.org/feeling-blue-at-st-emlyns/
http://www.rcemlearning.co.uk/modules/papa-smurf-has-a-seizure/
http://emergencymedicineireland.com/2011/07/why-methaemoglobinaemia-is-a-good-thing/
http://emergencymedicineireland.com/2011/07/why-methaemoglobinaemia-is-a-bad-thing/
Subscribe to:
Posts (Atom)













