We do back pain examination every day, but it is worth remembering how to do it properly.
- Introduction, Consent, Handwashing, Chaparone. Exposure from the waist up
- Inspection
Inspection from the back and side for:
Cervical lordosis, thoracic kyphosis and lumbar lordosis (lost with age, ank spond, acute disc prolapse).
Cafe au lait spots (neurofibromatosis), hairy patch (spinal dysraphism)
Muscle wasting
Scars
- Palpation
For temperature
Palpate each spinous process
Palpate sacroiliac joints
Palpate paraspinal muscles
Percuss with a fist or tendon hammer (infection, fracture or tumour)
- Move
Lumbar: Lumbar flexion, extension and lateral flexion.
run hands down side (lateral flexion)
touch their toes with knees straight (flexion)
lean backwards with knes straight (extension) - no extension in facet disease.
Can do a modified Schobers Test - place index and middle fingers 5 centimeters apart and noting how close and far apart they move on the movements.
C-Spine
Lateral flexion: place your ear on your shoulder;
rotation: look over your shoulder;
flexion: put your chin on your chest;
extension: put your head back to look at the ceiling.
Thoracic
Fix pelvis and turn
- Special Tests
Straight leg raise - to look for sciatica
Sciatic nerve test - do SLR. When pain brought on, dorsiflex the foot = positive = sciatic!
Bowstring test - SLR. Then lower. Apply popliteal compression = symptoms.
Femoral nerve stretch test - lie prone, passively flex knee - severe = positive.
Tiptoe test - tests S1
Duck walk (on heels) - for L4 power
Neurological examination
References
http://www.osceskills.com/e-learning/subjects/spine-examination/
Monday 26 September 2016
Thursday 22 September 2016
RSI
There are six separate phases of RSI.
1. Preoxygenation
Make sure you use your basic airway adjuncts as needed
Consider NODSAT
2. Preparation -
pre-assessment - use "LEMON" to see if you think the tube might be difficult
equipment - use a challenge and response checklist to make sure you have remembered everything, even capnography
position patient - find a pillow!
protect c-spine
3. Premedication
Fentanyl - onset 3 min, offset 20min
This can be useful in patients who have a head injury
4. Paralysis and Sedation
Paralysis -
Suxamethonium - depolarising. 1 - 1.5mg/kg bolus
10-20second onset with 3 - 5 minute offset
or Rocuronium - 1 - 1.5mg/kg
Hepatic and biliary excretion so longer offset time and longer onset time
Sedation
Propofol - 1.5 - 2.5mg/kg induction. Maintainence at 1-4 mg/kg/hr
15-20second onset, 5 - 10min offset
or Ketamine
We don't seem to use Thio or any of the others now.
5. Passage of the ETT - this is the very tricky bit that needs some theatre time!
6. Post intubation care
Complications of RSI
Failure to oxygenate - prevent by using checklist and DAS guidelines
Anaphylaxis - treat with anaphylaxis algorithm
Hypotension - turn down rate of sedation agent. Give small boluses of metaraminol or adrenaline IV to maintain BP.
Laryngospasm - oxygen, Larsens Notch
Apply PEEP
If this fails, paralyse and intubate (may be difficult)
Capnography
You need a good seal. If you have a poor trace this might be reflected in your capnography trace.
1. Preoxygenation
Make sure you use your basic airway adjuncts as needed
Consider NODSAT
2. Preparation -
pre-assessment - use "LEMON" to see if you think the tube might be difficult
equipment - use a challenge and response checklist to make sure you have remembered everything, even capnography
position patient - find a pillow!
protect c-spine
3. Premedication
Fentanyl - onset 3 min, offset 20min
This can be useful in patients who have a head injury
4. Paralysis and Sedation
Paralysis -
Suxamethonium - depolarising. 1 - 1.5mg/kg bolus
10-20second onset with 3 - 5 minute offset
or Rocuronium - 1 - 1.5mg/kg
Hepatic and biliary excretion so longer offset time and longer onset time
Sedation
Propofol - 1.5 - 2.5mg/kg induction. Maintainence at 1-4 mg/kg/hr
15-20second onset, 5 - 10min offset
or Ketamine
We don't seem to use Thio or any of the others now.
5. Passage of the ETT - this is the very tricky bit that needs some theatre time!
6. Post intubation care
Complications of RSI
Failure to oxygenate - prevent by using checklist and DAS guidelines
Anaphylaxis - treat with anaphylaxis algorithm
Hypotension - turn down rate of sedation agent. Give small boluses of metaraminol or adrenaline IV to maintain BP.
Laryngospasm - oxygen, Larsens Notch
Apply PEEP
If this fails, paralyse and intubate (may be difficult)
Capnography
You need a good seal. If you have a poor trace this might be reflected in your capnography trace.
Basic Airway Management
I hope we're pretty good at this!
Hands: head tilt chin lift or jaw thrust
Adjuncts: oropharyngeal airway -hard to hard preferred (middle of incisors to angle of jaw). Soft to soft (tragus to corner of mouth alternative)
nasopharyngeal 6mm women, 7mm men (not patient's little finger)
supraglottic airway eg. IGel
Tube: probably as an emergency RSI (see later)
Failed Intubation:
DAS Guidelines are really simple now and are easy to remember and follow.
Plan A: Intubate
Plan B: Supraglottic
Plan C: Facemask. Paralyse
Plan D: Front of neck surgical cric
Difficult BVM Assessment
M: Mask seal – for example a beard or blood
O: Obesity (BMI >30) and obstruction (snoring history)
A: Age >55
N: No teeth
S: Stiff lungs
Difficult Intubation Assessment
L: Look: a rapid ‘gut-feeling’ assessment
E: Evaluate the 3-3-2 rule
M: Mallampati score
O: Obesity/obstruction (stridor in particular is worrying)
N: Neck mobility
References and Further Links
http://learning.bmj.com/learning/modules/end/ELU.html?moduleId=10033823
https://www.das.uk.com/files/das2015intubation_guidelines.pdf
Hands: head tilt chin lift or jaw thrust
Adjuncts: oropharyngeal airway -hard to hard preferred (middle of incisors to angle of jaw). Soft to soft (tragus to corner of mouth alternative)
nasopharyngeal 6mm women, 7mm men (not patient's little finger)
supraglottic airway eg. IGel
Tube: probably as an emergency RSI (see later)
Failed Intubation:
DAS Guidelines are really simple now and are easy to remember and follow.
Plan A: Intubate
Plan B: Supraglottic
Plan C: Facemask. Paralyse
Plan D: Front of neck surgical cric
Difficult BVM Assessment
M: Mask seal – for example a beard or blood
O: Obesity (BMI >30) and obstruction (snoring history)
A: Age >55
N: No teeth
S: Stiff lungs
Difficult Intubation Assessment
L: Look: a rapid ‘gut-feeling’ assessment
E: Evaluate the 3-3-2 rule
M: Mallampati score
O: Obesity/obstruction (stridor in particular is worrying)
N: Neck mobility
References and Further Links
http://learning.bmj.com/learning/modules/end/ELU.html?moduleId=10033823
https://www.das.uk.com/files/das2015intubation_guidelines.pdf
Advanced Life Support
We all know how to manage cardiac arrest, as per ALS. There's always a few little things that I remember, and are good to remind ourselves of. There's also a few little things that we can do and think of as "extras".
Causes of Arrest
The 4Hs and 4Ts are commonly used, and this picture on the left (from Twitter, original source unknown) is a nice way of thinking about it.
Pyrexia must be prohibited post-cardiac arrest. It is common in the first 48 hours and the risk of a poor neurological outcome increases with each degree rise over 37oC. Maintain normothermia - 32 to 36 degrees.
If we have PEA, it is useful for us to think "Is it wide" or "is it narrow" to help us further hone our diagnostic reasoning.
Drugs
Post ROSC Care
A MAP of about 65-100 mmHg is a reasonable starting point in most –adjusted according to response.
"Special" Circumstances
Hypothermia: No adrenaline until >30,
double time in between 30 - 35,
normal once >35
Drugs are often ineffective and will undergo reduced metabolism.
In primary hypothermic cardiac arrest, death should not be confirmed until:
The patient has been re-warmed
Or
Other unsurvivable injuries have been identified
Or
Re-warming has failed despite all available measures
LA OD
Intralipid
1.5ml/kg bolus AND infusion 15ml/kg / hour
After 5 min 2 further boluses if not better
And double infusion to 30m/kg/hr
Resuscitate for one hour
Lidocaine toxicity
5 Light headedness, circumoral paraesthesia, slurred speech + tinnitus
10 Convulsions, LOC
15 Coma, myocardial depression
20 Resp arrest + arrhythmia
>25 Cardiac arrest
Pregnancy
Peri-mortem c-section
References and Links
http://rebelem.com/a-new-pulseless-electrical-activity-algorithm/
http://www.rcemlearning.co.uk/modules/an-unusual-cause-of-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/ooh-cardiac-arrest/
http://www.rcemlearning.co.uk/references/post-cardiac-arrest-care-of-the-rosc-patient/
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/management-of-post-arrest-patients-including-prognostication/
http://www.rcemlearning.co.uk/modules/a-systematic-review-of-therapeutic-hypothermia-for-non-shockable-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-hypothermic-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/modules/the-curious-incident-of-the-wolff-in-the-nighttime/
http://www.rcemlearning.co.uk/modules/the-resus-lottery/
http://www.rcemfoamed.co.uk/portfolio/saap-intra-aortic-adrenaline-in-cardiac-arrest/
Causes of Arrest
The 4Hs and 4Ts are commonly used, and this picture on the left (from Twitter, original source unknown) is a nice way of thinking about it.
Pyrexia must be prohibited post-cardiac arrest. It is common in the first 48 hours and the risk of a poor neurological outcome increases with each degree rise over 37oC. Maintain normothermia - 32 to 36 degrees.
If we have PEA, it is useful for us to think "Is it wide" or "is it narrow" to help us further hone our diagnostic reasoning.
Drugs
— Salim R. Rezaie (@srrezaie) September 29, 2015
Post ROSC Care
A MAP of about 65-100 mmHg is a reasonable starting point in most –adjusted according to response.
"Special" Circumstances
Hypothermia: No adrenaline until >30,
double time in between 30 - 35,
normal once >35
Drugs are often ineffective and will undergo reduced metabolism.
In primary hypothermic cardiac arrest, death should not be confirmed until:
The patient has been re-warmed
Or
Other unsurvivable injuries have been identified
Or
Re-warming has failed despite all available measures
LA OD
Intralipid
1.5ml/kg bolus AND infusion 15ml/kg / hour
After 5 min 2 further boluses if not better
And double infusion to 30m/kg/hr
Resuscitate for one hour
Lidocaine toxicity
5 Light headedness, circumoral paraesthesia, slurred speech + tinnitus
10 Convulsions, LOC
15 Coma, myocardial depression
20 Resp arrest + arrhythmia
>25 Cardiac arrest
Pregnancy
Peri-mortem c-section
http://rebelem.com/a-new-pulseless-electrical-activity-algorithm/
http://www.rcemlearning.co.uk/modules/an-unusual-cause-of-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/ooh-cardiac-arrest/
http://www.rcemlearning.co.uk/references/post-cardiac-arrest-care-of-the-rosc-patient/
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/management-of-post-arrest-patients-including-prognostication/
http://www.rcemlearning.co.uk/modules/a-systematic-review-of-therapeutic-hypothermia-for-non-shockable-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-hypothermic-cardiac-arrest/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/modules/the-curious-incident-of-the-wolff-in-the-nighttime/
http://www.rcemlearning.co.uk/modules/the-resus-lottery/
http://www.rcemfoamed.co.uk/portfolio/saap-intra-aortic-adrenaline-in-cardiac-arrest/
Anaphylaxis
Anaphylaxis is not common, but as prompt treatment is so essential we need to know about it. It's similar in children (covered here) and adults.
Biphasic response occurs in 20% - much debate now about whether or not we need to observe people.
Causes
Antibiotics, especially penicillin
Aspirin
NSAIDs (the second most common cause of drug induced anaphylaxis)
Angiotensin Converting Enzyme Inhibitors
Treatment
Resus Council Algorithm
- Bue needle to inject adrenaline – orange is too short.
- IM injection in the anterolateral aspect of the thigh is best – it is absorbed quicker here than in the deltoid.
- No evidence to support use of H1 antihistamines in anaphylaxis (Sheikh et al 2007). Some evidence of improved skin signs e.g. itching for less severe reactions. Important to remember they can also cause drowsiness, confusion, fatigue and dizziness as side effects.
- H2-antihistamines = no evidence to support their routine use in anaphylaxis (Nurmatov et al 2014). May provide some relief for less emergent skin symptoms.
- Steroids (glucocorticoids) = no evidence to support their routine use in anaphylaxis (Choo et al 2012). The primary reason for administration has been to prevent biphasic reactions (see below), however a recent paper by Grunau et al (2015) found they were not associated with decreased relapses within 7 days.
Investigations
Tryptase sensitivity is low – 21%, especially to foods. It's not recommended in children.
Check tryptase as soon as resuscitation has started, 1-2 hours after symptoms, 24 hours later or in convalescence (some people have raised baseline tryptase levels).
"Special" Anaphylaxis
 Hereditary Angioedema
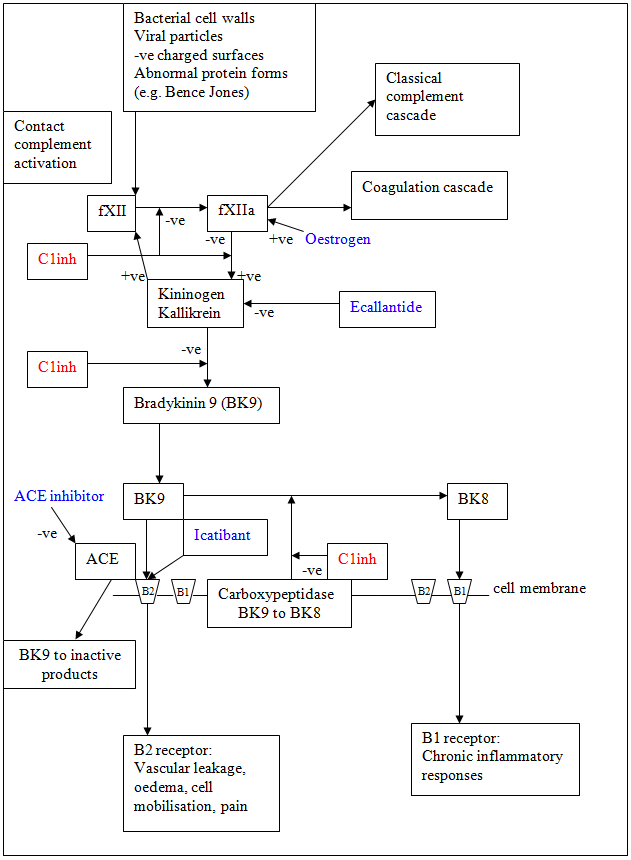
Hereditary AngioedemaOften doesn't respond to initial treatment. There's a good picture on RCEMLearning that shows how bradykinin is produced, both from ACE and oestrogen - and this can cause oedema.
Treat with concentrations of plasma and recombinant derived C1 inhibitor, or FFP if that isn't available.
Tranexamic acid may be helpful.
ACE Inhibitor
Excessive accumulation of bradykinin. Usually occurs soon after starting ACEi, but may be years later. Higher incidence amongst women, and African Americans.
It tends to be slowly evolving, with no urticarial or itching. Starts with focal, often asymmetric swelling.
Manage similar to C1 esterase inhibitor deficiency – give some FFP.
Kounis Syndrome
Anaphylaxis of the coronary arteries – maybe with or without existing coronary disease. There are lots of mast cells in the coronary arteries of people with coronary artery diseases. Coronary vasospasm is induced. There are no guidelines on how to treat it!
References and Further Reading
http://www.rcemlearning.co.uk/modules/anaphylaxis-induced-cardiac-arrest/
http://www.rcemlearning.co.uk/modules/anaphylaxis/pre-test/
http://www.rcemlearning.co.uk/references/cardiac-arrest-in-special-circumstances-anaphylaxis/
http://www.rcemlearning.co.uk/references/anaphylaxis/
http://www.rcemlearning.co.uk/references/hereditary-angioedema/
http://calgaryguide.ucalgary.ca/type-i-hypersensitivity-pathogenesis-and-clinical-findings/
http://lifeinthefastlane.com/anaphylaxis-amplification/
http://thesgem.com/2013/12/sgem57-should-i-stay-or-should-i-go-biphasic-anaphylactic-response/
http://coreem.net/journal-reviews/biphasic-reactions-in-emergency-department-patients-with-allergic-reactions-or-anaphylaxis/
http://www.ncbi.nlm.nih.gov/pubmed/24239340
https://www.resus.org.uk/anaphylaxis/emergency-treatment-of-anaphylactic-reactions/
http://secure.rcem.ac.uk/code/document.asp?ID=5072
http://kcgs/Documents/CDUPruh013.pdf
http://kcgs/Documents/CDU002.pdf
emergencymedicinecases.com/anaphylaxis-anaphylactic-shock/
http://paediatricem.blogspot.co.uk/2013/07/anaphylaxis_29.html
Subscribe to:
Posts (Atom)



