"Widespread and inappropriate activation of the coagulation and fibrinolytic systems". Either bleeding (65%) or thrombosis predominates. This can be caused by a variety of reasons:
- Infection
Most common cause of DIC, normally bleeding
10%–20% of patients with gram-neg sepsis have DIC
- Carcinoma
DIC is often chronic and compensated, normally thrombosis.
- Leukemia
More likely to have bleeding than thrombosis
- Trauma
- Liver disease
May have chronic compensated DIC, or acute.
- Pregnancy complications
- Envenomation
- ARDS
20% of patients with ARDS develop DIC; 20% of patients with DIC develop ARDS
- Transfusion reactions
Diagnoses
Acute DIC
Platelets low (or dropping) - sensitive, not specific
PT prolonged
Fibrinogen low
<100 correlates w/ severe DIC
PTT prolonged
D-dimer elevated - sensitive, not specific
RBCs fragmented (not specific)
Chronic DIC
FDP: Elevated
D-dimer: Elevated
Platelet: Variable
Fibrinogen: Normal-elevated
PT: Normal
PTT: Normal
RBCs: Fragmented
Consider an LDH - it is released by red cells. It's a good indicator there are likely to be rbc fragments
Differential Diagnoses TTP-HUS: Patients usually have little or no prolongation of PT or PTT
Severe liver disease: d-dimer only mildly elevated
Heparin-induced thrombocytopenia
Treatment Treat underlying illness
Bloods ++++++ - haematology need them to work out what's going on. Include fibrinogen.
Haematology advice for cryoprecipitate, platelets, FFP, vitamin K, folate, heparin
References
http://www.wikem.org/wiki/DIC_%28Disseminated_Intravascular_Coagulation%29
http://lifeinthefastlane.com/tag/dic/
http://lifeinthefastlane.com/education/ccc/disseminated-intravascular-coagulation/
http://wikemerg.ca/wiki/coagulopathy-dic
http://lifeinthefastlane.com/?attachment_id=7802
http://resus.me/guidelines-for-d-i-c/
Wednesday, 30 April 2014
Sunday, 27 April 2014
Headache
Headache is a massive subject to try and cover. One website nicely splits them into three main groups - so I'll go over headache in each of these groups...
Common
Migraine Headache
Tension Headache
Cluster Headache
Killers
Meningitis/encephalitis
SAH / sentinel bleed
Intracranial Hemorrhage (ICH) (subdura/epidural)
Acute obstructive hydrocephalus (and blocked shunts)
Space occupying lesions
CVA
CO Poisoning
Basilar artery dissection
Preeclampsia
Cerebral Venous Thrombosis (pregnancy/post-partum)
Brain abscess
Maimers
Temporal Arteritis (>50yrs & ESR)
Idiopathic Intracranial Hypertension (pseudotumor cerebri)
Acute glaucoma
Acute sinusitis
References
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1559
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1553
http://learning.bmj.com/learning/module-intro/tricyclic-antidepressants-headaches.html?moduleId=10017236&searchTerm=%E2%80%9Cheadache%E2%80%9D&page=1&locale=en_GB
http://jnnp.bmj.com/content/72/suppl_2/ii33.full
http://embasic.org/2011/08/27/headache/
http://wikem.org/wiki/Headache
http://emeddoc.org/?p=481
http://flippedemclassroom.wordpress.com/category/headache/
http://lifeinthefastlane.com/education/symptoms/headache/
http://secure.collemergencymed.ac.uk/code/document.asp?ID=5074
http://guidance.nice.org.uk/CG150
http://www.sign.ac.uk/guidelines/fulltext/107/
Misc. Headaches
Benign Inter-cranial Hypertension
This is caused by raised CSF pressure, often in middle aged, obese females. It is occasional associated with a VI nerve palsy. It can be caused by SLE, CRF, endocrine problems. Also known as pseusotumour cerebri.
Symptoms:
Frontal headache, worse on lying down or stooping, night waking.
Can exacerbate migraines.
Lethargy, tiredness. Get papiloedema.
Investigations:
Need CT and MRI.
Treatment
Acetazolamide can help. Steroids in first two weeks LP shunt.
Management
Need to monitor vision
Antimigraine treatment may help.
Trigeminal Neuralgia
Stabbing unilateral pain. Treat with carbamazepine and oral analgesia. Admit if pain severe.

Space-occupying Lesion
Consider if headache always on same side. Dull, aching and headaches made worse by lying down or straining.
Central venous thrombosis
Presents similarly to SAH. May be associated with sinus infections, pregnancy and the post-partum period. May be missed on CT, but a clue would be raised intracranial pressure at LP.
Thunderclap Headache
several other potential vascular causes of thunderclap headache, other than SAH and these include:
cerebral venous thrombosis
arterial dissection
ischaemic or haemorrhagic stroke
intracerebral, intraventricular, extradural or subdural haemorrhage
vasculitides
reversible cerebral vasoconstriction syndrome
Pituitary Apoplexy
Occurs in 5% of patients with a pituitary tumour, and for 80% of patients is the first presentation of the tumour. Sudden onset headache, vomiting, visual impairment and decreased consciousness. Think about if headache + eye signs.
Brain Abscess
Toxoplasma gondii is an intracellular parasite that infects birds and mammals. Its definitive host is the cat. Excretion of oocytes in its faecal content followed by human contaminated uncooked consumption can lead to human infection. In immunocompetent individuals, it primarily causes a subclinical or asymptomatic infection. In immunocompromised individuals (e.g. AIDS patients), toxoplasmosis is the most common cause of a brain abscess.
http://m.adc.bmj.com/content/78/1/89.full http://radiopaedia.org/articles/idiopathic-intracranial-hypertension-1
http://radiopaedia.org/cases/benign-intracranial-hypertension-3
http://annals.org/article.aspx?articleid=
http://radiopaedia.org/articles/dural_venous_sinus_thrombosis
http://radiopaedia.org/articles/cerebral-venous-thrombosis
This is caused by raised CSF pressure, often in middle aged, obese females. It is occasional associated with a VI nerve palsy. It can be caused by SLE, CRF, endocrine problems. Also known as pseusotumour cerebri.
Symptoms:
Frontal headache, worse on lying down or stooping, night waking.
Can exacerbate migraines.
Lethargy, tiredness. Get papiloedema.
Investigations:
Need CT and MRI.
Treatment
Acetazolamide can help. Steroids in first two weeks LP shunt.
Management
Need to monitor vision
Antimigraine treatment may help.
Trigeminal Neuralgia
Stabbing unilateral pain. Treat with carbamazepine and oral analgesia. Admit if pain severe.

Space-occupying Lesion
Consider if headache always on same side. Dull, aching and headaches made worse by lying down or straining.
Central venous thrombosis
Presents similarly to SAH. May be associated with sinus infections, pregnancy and the post-partum period. May be missed on CT, but a clue would be raised intracranial pressure at LP.
Thunderclap Headache
several other potential vascular causes of thunderclap headache, other than SAH and these include:
cerebral venous thrombosis
arterial dissection
ischaemic or haemorrhagic stroke
intracerebral, intraventricular, extradural or subdural haemorrhage
vasculitides
reversible cerebral vasoconstriction syndrome
Pituitary Apoplexy
Occurs in 5% of patients with a pituitary tumour, and for 80% of patients is the first presentation of the tumour. Sudden onset headache, vomiting, visual impairment and decreased consciousness. Think about if headache + eye signs.
Brain Abscess
Thinking about these headache causing diseases when it comes down to a patient with HIV/AIDS. #FOAMED #aceprecap13 pic.twitter.com/O6F6Xe20JV
— FOAMed NL (@FOAMedNL) November 22, 2013Toxoplasma gondii is an intracellular parasite that infects birds and mammals. Its definitive host is the cat. Excretion of oocytes in its faecal content followed by human contaminated uncooked consumption can lead to human infection. In immunocompetent individuals, it primarily causes a subclinical or asymptomatic infection. In immunocompromised individuals (e.g. AIDS patients), toxoplasmosis is the most common cause of a brain abscess.
http://m.adc.bmj.com/content/78/1/89.full http://radiopaedia.org/articles/idiopathic-intracranial-hypertension-1
http://radiopaedia.org/cases/benign-intracranial-hypertension-3
http://annals.org/article.aspx?articleid=
http://radiopaedia.org/articles/dural_venous_sinus_thrombosis
http://radiopaedia.org/articles/cerebral-venous-thrombosis
http://radiopaedia.org/articles/brain-abscess-1
http://radiopaedia.org/cases/brain-abscess-1
http://ermentor.com/2013/10/does-that-hiv-infected-patient-with-a-headache-really-require-that-ct-head/
http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2013.187.1_MeetingAbstracts.A2958
http://radiopaedia.org/articles/cerebral-toxoplasmosis-2
http://lifeinthefastlane.com/education/ccc/toxoplasmosis/
http://radiopaedia.org/cases/brain-abscess-1
http://ermentor.com/2013/10/does-that-hiv-infected-patient-with-a-headache-really-require-that-ct-head/
http://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2013.187.1_MeetingAbstracts.A2958
http://radiopaedia.org/articles/cerebral-toxoplasmosis-2
http://lifeinthefastlane.com/education/ccc/toxoplasmosis/
Blocked VP Shunts
Normal Patho-physiology
- CSF produced at 0.35 ml/min (20 ml/hour or 500 ml/24 hours)
- Recycled over three times each day
- Capacity of normal lateral and third ventricles is approximately 20 ml
- ICP rises if production of CSF exceeds absorption. CSF production falls as ICP increases.
Shunts
Most shunting systems drain according to the differential pressure gradient between the ventricle and the tip of the distal catheter. Most neurosurgeons use medium pressure valves, that will drain CSF continuously if the differential pressure is over about 10 mm Hg. The ventricular catheter of a shunt is normally inserted through a burr-hole in the right parieto-occipital region and the valve will sit usually behind the right ear. The distal catheter is tunnelled subcutaneously down to another incision in the abdomen where it is then placed into the peritoneal cavity. It is not usually helpful for non-neurosurgeons to palpate or flush the shunt valve, as their contours and characteristics are so variable as to make interpretation notoriously inaccurate.
Blocked shunts:
blood or debris in the proximal site (choroid plexus within the ventricle can get stuck in it
fracture of the tubing along its course
infection of the tubing along its course
something like a piece of omentum getting stuck in the distal port in the abdomen
Hydrocephalus features
Young adults:
- Symptoms—headache, vomiting, failing vision, drowsiness, “muzziness of the head”, fatigue
- Signs—papilloedema, enlarged blind spots on visual field analysis or reduced visual acuity, failure of upward gaze, general clumsiness, dyspraxic gait, large head
Older adults/elderly:
- Symptoms—slowing of mental capacity, unsteady on feet/frequent falls, incontinence, drowsiness, headaches less frequently
- Signs—gait dyspraxia (slow, hesitant shuffling gait), dementia (reduced mini-mental score), rarely papilloedema
Clinical features of shunt malfunction:
Drowsiness and general malaise
Headaches
Vomiting
Papilloedema with or without failing vision
Occasionally failure of upward gaze
Neck stiffness
Thoracic back pain in patients with spina bifida
Abdominal tenderness or distension
Investigations
CT scan has sensitivity of 80% and shunt series (plain films of neck and abdo) has sens of 20% but you still need both.
Head CT (to help define if there is hydrocephalus vs overdrainage)
Shunt Series (to image the apparatus for obvious kinks and breaks)Peripheral blood for C reactive protein, white cell count if there has been any recent surgery
ICP monitoring/lumbar infusion test
http://jnnp.bmj.com/content/73/suppl_1/i17.full
http://adc.bmj.com/content/87/3/198
http://emergencymedicineireland.com/2012/04/raised-icp-and-intracranial-shunts-some-notes/
http://pedemmorsels.com/tapping-a-vp-shunt/
- CSF produced at 0.35 ml/min (20 ml/hour or 500 ml/24 hours)
- Recycled over three times each day
- Capacity of normal lateral and third ventricles is approximately 20 ml
- ICP rises if production of CSF exceeds absorption. CSF production falls as ICP increases.
Shunts
Most shunting systems drain according to the differential pressure gradient between the ventricle and the tip of the distal catheter. Most neurosurgeons use medium pressure valves, that will drain CSF continuously if the differential pressure is over about 10 mm Hg. The ventricular catheter of a shunt is normally inserted through a burr-hole in the right parieto-occipital region and the valve will sit usually behind the right ear. The distal catheter is tunnelled subcutaneously down to another incision in the abdomen where it is then placed into the peritoneal cavity. It is not usually helpful for non-neurosurgeons to palpate or flush the shunt valve, as their contours and characteristics are so variable as to make interpretation notoriously inaccurate.
Blocked shunts:
blood or debris in the proximal site (choroid plexus within the ventricle can get stuck in it
fracture of the tubing along its course
infection of the tubing along its course
something like a piece of omentum getting stuck in the distal port in the abdomen
Hydrocephalus features
Young adults:
- Symptoms—headache, vomiting, failing vision, drowsiness, “muzziness of the head”, fatigue
- Signs—papilloedema, enlarged blind spots on visual field analysis or reduced visual acuity, failure of upward gaze, general clumsiness, dyspraxic gait, large head
Older adults/elderly:
- Symptoms—slowing of mental capacity, unsteady on feet/frequent falls, incontinence, drowsiness, headaches less frequently
- Signs—gait dyspraxia (slow, hesitant shuffling gait), dementia (reduced mini-mental score), rarely papilloedema
Clinical features of shunt malfunction:
Drowsiness and general malaise
Headaches
Vomiting
Papilloedema with or without failing vision
Occasionally failure of upward gaze
Neck stiffness
Thoracic back pain in patients with spina bifida
Abdominal tenderness or distension
Investigations
CT scan has sensitivity of 80% and shunt series (plain films of neck and abdo) has sens of 20% but you still need both.
Head CT (to help define if there is hydrocephalus vs overdrainage)
Shunt Series (to image the apparatus for obvious kinks and breaks)Peripheral blood for C reactive protein, white cell count if there has been any recent surgery
ICP monitoring/lumbar infusion test
http://jnnp.bmj.com/content/73/suppl_1/i17.full
http://adc.bmj.com/content/87/3/198
http://emergencymedicineireland.com/2012/04/raised-icp-and-intracranial-shunts-some-notes/
http://pedemmorsels.com/tapping-a-vp-shunt/
Saturday, 26 April 2014
Glaucoma
Glaucoma is listed in the headache syllabus, but no-where else. It's implied in the red eye syllabus.
Epidemiology
- Affects 2% of over 40 years old
- Up to 10% of those above 80 years.
- Second most common cause of blindness in the UK
- Accounts for 10% of registrable blindness.
Pathopysiology
There are two types of glaucoma - open or closed. The "angle" in open-angle glaucoma refers to the angle between the iris and the cornea.

Closed-angle glaucoma occurs when the iridocorneal angle narrows so much that the aqueous fluid is unable to flow from the posterior to the anterior chamber and cannot reach the trabecular meshwork.
Open-angle glaucoma tends to progress at a slower rate than closed-angle glaucoma, and patients may not realise they have vision loss until there has been irreversible damage to the optic nerve and retinal nerve fibres. Acutely, closed-angle glaucoma is much more important to know about.
Risk factors include:
- history of previous episodes recent use of anticholinergic drugs
- African or Afro-Carribean origin Chinese, Hispanic and Inuit origin
- ocular hypertension (OHT)
- increasing age
- short sightedness (myopia)
- family history
- diabetes
Symptoms
- acute onset of a red and painful eye
- impaired vision
- multicoloured haloes (like a rainbow) forming around lights
- nausea, vomiting and headache
The acute attack can be preciptated by:
- topical mydriatics anticholinergic and sympathomimetic drugs
- emotional stimuli
- accommodation (e.g. reading)
- dim light
Treatment
There are five main drug classes of glaucoma eye drops:
- prostaglandin derivatives beta-blockers carbonic anhydrase inhibitors
- sympathomimetics miotics
- head up at least 30 degrees
- symptomatic treatment of pain and nausea/ vomiting
- discontinue any precipitants and treat underlying causes
It is controversial whether to start treatment in the ED or not. I suspect it depends on transfer time to ophthalmology assessment. Consider opiate analgesia, an antiemetic and acetazolamide 500mg IV then 500mg PO. Treatment with a topical miotic such as pilocarpine 1 or 2% every 5 minutes should be started approximately 1 hour after commencing other measures as initially the pupil is usually paralysed and unresponsive.
References
http://www.enlightenme.org/knowledge-bank/cempaedia/atraumatic-red-eye
http://www.enlightenme.org/learning-zone/under-pressure
http://www.enlightenme.org/knowledge-bank/cempaedia/eye-initial-assessment
http://www.ophthobook.com/chapters/glaucoma
http://learning.bmj.com/learning/module-intro/glaucoma-chronic-open-angle-glaucoma-ocular-hypertension-diagnosis-management-.html?moduleId=10013290&searchTerm=%E2%80%9Cglaucoma%E2%80%9D&page=1&locale=en_GB
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1350
http://lifeinthefastlane.com/ophthalmology-befuddler-007-2/
Epidemiology
- Affects 2% of over 40 years old
- Up to 10% of those above 80 years.
- Second most common cause of blindness in the UK
- Accounts for 10% of registrable blindness.
Pathopysiology
There are two types of glaucoma - open or closed. The "angle" in open-angle glaucoma refers to the angle between the iris and the cornea.

Closed-angle glaucoma occurs when the iridocorneal angle narrows so much that the aqueous fluid is unable to flow from the posterior to the anterior chamber and cannot reach the trabecular meshwork.
Open-angle glaucoma tends to progress at a slower rate than closed-angle glaucoma, and patients may not realise they have vision loss until there has been irreversible damage to the optic nerve and retinal nerve fibres. Acutely, closed-angle glaucoma is much more important to know about.
Risk factors include:
- history of previous episodes recent use of anticholinergic drugs
- African or Afro-Carribean origin Chinese, Hispanic and Inuit origin
- ocular hypertension (OHT)
- increasing age
- short sightedness (myopia)
- family history
- diabetes
Symptoms
- acute onset of a red and painful eye
- impaired vision
- multicoloured haloes (like a rainbow) forming around lights
- nausea, vomiting and headache
The acute attack can be preciptated by:
- topical mydriatics anticholinergic and sympathomimetic drugs
- emotional stimuli
- accommodation (e.g. reading)
- dim light
Treatment
There are five main drug classes of glaucoma eye drops:
- prostaglandin derivatives beta-blockers carbonic anhydrase inhibitors
- sympathomimetics miotics
- head up at least 30 degrees
- symptomatic treatment of pain and nausea/ vomiting
- discontinue any precipitants and treat underlying causes
It is controversial whether to start treatment in the ED or not. I suspect it depends on transfer time to ophthalmology assessment. Consider opiate analgesia, an antiemetic and acetazolamide 500mg IV then 500mg PO. Treatment with a topical miotic such as pilocarpine 1 or 2% every 5 minutes should be started approximately 1 hour after commencing other measures as initially the pupil is usually paralysed and unresponsive.
References
http://www.enlightenme.org/knowledge-bank/cempaedia/atraumatic-red-eye
http://www.enlightenme.org/learning-zone/under-pressure
http://www.enlightenme.org/knowledge-bank/cempaedia/eye-initial-assessment
http://www.ophthobook.com/chapters/glaucoma
http://learning.bmj.com/learning/module-intro/glaucoma-chronic-open-angle-glaucoma-ocular-hypertension-diagnosis-management-.html?moduleId=10013290&searchTerm=%E2%80%9Cglaucoma%E2%80%9D&page=1&locale=en_GB
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1350
http://lifeinthefastlane.com/ophthalmology-befuddler-007-2/
Monday, 21 April 2014
Subarachnoid Haemorrhage
SAH - the most feared cause of headache. Syncope + headache = think SAH.
Anatomy
Most SAHs occur in the circle of Willis - as this is where the brain gets its blood supply from.
Autosomal dominant polycystic kidney disease
Pseudoxanthoma elasticum
Ehler-Danlos syndrome type IV.
SAH:
1-7% of all strokes.
More common in young men than young women
Overall, more common in women.
Aspirin increases the mortality if it bleeds
Anatomy
Most SAHs occur in the circle of Willis - as this is where the brain gets its blood supply from.
There are two types of aneurysm with slightly different pathophysiology behind them.
Saccular Aneurysms: Approximately 90%, with high morbidity and mortality. The internal elastic membrane weakens, at the site of vessel bifurcation where blood flow is most turbulent.
Fusiform Aneurysms: These develop from ectatic, tortuous cerebral arteries, most often in the vertebrobasilar system. Patients with fusiform aneurysms characteristically present with symptoms of cranial-nerve or brainstem compression, but the symptoms are not commonly associated with subarachnoid hemorrhage.
Fusiform Aneurysms: These develop from ectatic, tortuous cerebral arteries, most often in the vertebrobasilar system. Patients with fusiform aneurysms characteristically present with symptoms of cranial-nerve or brainstem compression, but the symptoms are not commonly associated with subarachnoid hemorrhage.
Epidemiology
Screening is not beneficial, even in those with first degree relative history. If screening is appropriate, cranial MRA is used.
Aneursyms:
NOT Congenital - increased risk if first degree relative has SAH
With 2 relatives, 10 year risk of 7.1% versus 0.8%
Occur in about 1 in 40 people (1-5%).
Most never rupture.
Multiple aneurysms in 30%.
Berry aneuryms have increased rate of formation in:Occur in about 1 in 40 people (1-5%).
Most never rupture.
Multiple aneurysms in 30%.
Autosomal dominant polycystic kidney disease
Pseudoxanthoma elasticum
Ehler-Danlos syndrome type IV.
SAH:
1-7% of all strokes.
More common in young men than young women
Overall, more common in women.
Aspirin increases the mortality if it bleeds
Oestrogen deficiency (post - menopausal) raises the risk.
Hypertension
Smoking
Sympathomimetic drugs (phenylephrine and cocaine)
Diagnosis
Missed in 1/4 of patients as characteristic headache not present.
50% of patients rebleed within six months of the presentation
After that, 3% per year thereafter
Even in these patients, the possibility of having an intracranial aneurysm is low and screening all patients is not required in the absence of a positive family history. Cranial MRA is the imaging method of choice for screening.
Clinical Presentation - the Headache
Classically Instantaneous:
Instantaneous – 50%
2-60 seconds – 24%
1-5 minutes – 19%
No idea/unable to remember – 9%
1 hour has been suggested. The typical duration is of the order of 1-2 weeks.
Instantaneous – 50%
2-60 seconds – 24%
1-5 minutes – 19%
No idea/unable to remember – 9%
1 hour has been suggested. The typical duration is of the order of 1-2 weeks.
Features
Pancephalic
Lateralised in one third of patients
Sentinel Bleed:
No medical attention sout, or one missed.
No medical attention sout, or one missed.
Present in 30 - 50%
The classic headache, caused by aneurysmal rupture, release of blood, and raised ICP, happens in 97% of patients. Only around 25% of patients who visit A&E with this sudden severe headache (so called, “the worst headache of my life”) have acute subarachnoid haemorrhage. In only 12% of them, headache is the only complaint.
Clinical Features - other
Vomiting is not predictive but present in 75%
Seizure at onset (74%)
Reduced level of consciousness in 2/3 of people
Transient loss of consciousness in 26%
Delirium (1%)
Delirium (1%)
Focal neurology (15%)
3rd nerve palsy due to an aneurysm in the posterior communicating artery.
1 in 7 will have intraocular haemorrhages.
Ischaemic changes (of any type) on ECGare common
3rd nerve palsy due to an aneurysm in the posterior communicating artery.
1 in 7 will have intraocular haemorrhages.
Ischaemic changes (of any type) on ECGare common
Neck stiffness may develop – but usually only after several hours and is due to an inflammatory reaction to the blood in the subarachnoid space, and it may not develop at all if there’s only a small amount of blood.
Imaging
CXR: neurogenic pulmonary oedema
CTH: 90% sensitive within 24 hrs, 50% @ 72 hrs, detects hydrocephalus
CTA: assesses vascular anatomy
DSA: gold standard for diagnosis, allows intervention
MRI: mostly used for detection of AVM
CTH: 90% sensitive within 24 hrs, 50% @ 72 hrs, detects hydrocephalus
CTA: assesses vascular anatomy
DSA: gold standard for diagnosis, allows intervention
MRI: mostly used for detection of AVM
CT:
98% sensitivity if scanned within 12 hours of onset.
93% within 24 hours.
50% at 5 days – based on study from 1984.
Sensitivities unlikely to improve because small bleeds will be flushed away by normal CSF flow. There may not be enough blood present to appear as hyperdense to CSF on scanning.
98% sensitivity if scanned within 12 hours of onset.
93% within 24 hours.
50% at 5 days – based on study from 1984.
Sensitivities unlikely to improve because small bleeds will be flushed away by normal CSF flow. There may not be enough blood present to appear as hyperdense to CSF on scanning.
Angiography:
Cerebral angiography within 48-72 hours of the initial event.
Lumbar Puncture
1 in 10 of patients presenting with thunderclap headaches will have had a subarachnoid haemorrhage.
A non-contrast CT within 12 hours of onset of pain is 98% sensitive for detecting SAH.
Therefore the risk of missing a SAH may be as low as 2 in 1000 if the patient has had a negative CT in this timeframe.
Xanthochromia A fancy way of saying ‘Yellow colour’! - Bilirubin
96% sensitive if done 12 hours post headache
Positive for at least 2 weeks (possibly up to 4 weeks)
Other Investigations
ECG: tall peaked T waves, ST depression, prolonged QT, arrhythmia
Echo: neurogenic cardiomyopathy
Hyponatraemia + hypovolaemia from SAIDH or cerebral salt wasting -> worsens vasopasm
Troponin rise due to cardiomyopathy
Magnesium - may be low, poor prognosis.
Treatment
Supportive care as appropriate
Neurosurgery - surgical clipping or coil
Treat seizures (occur in 18% of patients) with benzodizepines and load with phenytoin 18 mg/kg IV
Prevent vasospasm - Nimodipine
(calcium channel antagonist with some selectivity for cerebral circulation)
Lower the SBP to below 140 mm Hg to help reduce the risk of rebleeding using intravenous labetalol. Avoid
vasodilators, such as nitroglycerin and sodium nitroprusside, because they increase the intracranial blood volume and intracranial pressure
If your patient is unconscious, you should not try to lower their blood pressure, at least temporarily
Anti-fibrinolytics, e.g. tranexamic acid
— controversial
— may reduce risk of re-bleed but increase risk of VTE
— some centers give until aneurysm is secured if no VTE risk factors, monitor for DVT
Treat fever - occurs in 70% of SAH and requires aggressive control. Look for and treat infection. Antipyretics.
3% will have a cardiac arrest. Aggressive resuscitation is essential as they appear to have a high rate of ROSC and half of the survivors will regain independent living.
Prognosis
Rebleeding - 24 to six hours
Vasospasm - 3 days to 2 weeks
Lumbar Puncture
1 in 10 of patients presenting with thunderclap headaches will have had a subarachnoid haemorrhage.
A non-contrast CT within 12 hours of onset of pain is 98% sensitive for detecting SAH.
Therefore the risk of missing a SAH may be as low as 2 in 1000 if the patient has had a negative CT in this timeframe.
Xanthochromia A fancy way of saying ‘Yellow colour’! - Bilirubin
96% sensitive if done 12 hours post headache
Positive for at least 2 weeks (possibly up to 4 weeks)
Other Investigations
ECG: tall peaked T waves, ST depression, prolonged QT, arrhythmia
Echo: neurogenic cardiomyopathy
Hyponatraemia + hypovolaemia from SAIDH or cerebral salt wasting -> worsens vasopasm
Troponin rise due to cardiomyopathy
Magnesium - may be low, poor prognosis.
Treatment
Supportive care as appropriate
Neurosurgery - surgical clipping or coil
Treat seizures (occur in 18% of patients) with benzodizepines and load with phenytoin 18 mg/kg IV
Prevent vasospasm - Nimodipine
(calcium channel antagonist with some selectivity for cerebral circulation)
Lower the SBP to below 140 mm Hg to help reduce the risk of rebleeding using intravenous labetalol. Avoid
vasodilators, such as nitroglycerin and sodium nitroprusside, because they increase the intracranial blood volume and intracranial pressure
If your patient is unconscious, you should not try to lower their blood pressure, at least temporarily
Anti-fibrinolytics, e.g. tranexamic acid
— controversial
— may reduce risk of re-bleed but increase risk of VTE
— some centers give until aneurysm is secured if no VTE risk factors, monitor for DVT
Treat fever - occurs in 70% of SAH and requires aggressive control. Look for and treat infection. Antipyretics.
3% will have a cardiac arrest. Aggressive resuscitation is essential as they appear to have a high rate of ROSC and half of the survivors will regain independent living.
Prognosis
Rebleeding - 24 to six hours
Vasospasm - 3 days to 2 weeks
Death - within three weeks after subarachnoid haemorrhage. 40 - 50% of patients die.
Dependent - in a third of survivors
Hunt and Hess grading
Grade 0: Unruptured aneurysm without symptoms.
Grade 1: Asymptomatic or minimal headache and slight nuchal rigidity (1% mortality).
Grade 1a: No acute meningeal or brain reaction, but with fixed neurological deficit.
Grade 2: Moderate-to-severe headache, nuchal rigidity, no neurological deficit other than cranial nerve palsy (5% mortality).
Grade 3: Drowsy, confused or mild focal deficit (19% mortality).
Grade 4: Stupor, moderate-to-severe hemiparesis, possible early decerebrate rigidity and vegetative disturbances (42% mortality).
Grade 5: Deep coma, decerebrate rigidity, moribund appearance (77% mortality).
If there is a co-existing serious illness, this adds a grade.
Grade 0: Unruptured aneurysm without symptoms.
Grade 1: Asymptomatic or minimal headache and slight nuchal rigidity (1% mortality).
Grade 1a: No acute meningeal or brain reaction, but with fixed neurological deficit.
Grade 2: Moderate-to-severe headache, nuchal rigidity, no neurological deficit other than cranial nerve palsy (5% mortality).
Grade 3: Drowsy, confused or mild focal deficit (19% mortality).
Grade 4: Stupor, moderate-to-severe hemiparesis, possible early decerebrate rigidity and vegetative disturbances (42% mortality).
Grade 5: Deep coma, decerebrate rigidity, moribund appearance (77% mortality).
If there is a co-existing serious illness, this adds a grade.
The Ottawa Sub-Arachoid Rule
For alert patients older than 15 y with new severe nontraumatic headache reaching maximum intensity
within 1 h. Not for patients with new neurologic deficits, previous aneurysms, SAH, brain tumors, or history of recurrent headaches (=3 episodes over the course of =6 mo)
Investigate if 1 or more high-risk variables present:
- Age =40 y
- Neck pain or stiffness
- Witnessed loss of consciousness
- Onset during exertion
- Thunderclap headache (instantly peaking pain)
- Limited neck flexion on examination
within 1 h. Not for patients with new neurologic deficits, previous aneurysms, SAH, brain tumors, or history of recurrent headaches (=3 episodes over the course of =6 mo)
Investigate if 1 or more high-risk variables present:
- Age =40 y
- Neck pain or stiffness
- Witnessed loss of consciousness
- Onset during exertion
- Thunderclap headache (instantly peaking pain)
- Limited neck flexion on examination
References
http://www.enlightenme.org/learning-zone/grading-subarachnoid-haemorrhage
http://www.aafp.org/afp/2002/0815/p601.html
http://learning.bmj.com/learning/module-intro/subarachnoid-haemorrhage-diagnosis-management.html?moduleId=10022933&searchTerm=%E2%80%9Csubarachnoid%E2%80%9D&page=1&locale=en_GB
http://www.bmj.com/content/341/bmj.c5204?sso=
http://www.aafp.org/afp/2002/0815/p601.html
http://learning.bmj.com/learning/module-intro/subarachnoid-haemorrhage-diagnosis-management.html?moduleId=10022933&searchTerm=%E2%80%9Csubarachnoid%E2%80%9D&page=1&locale=en_GB
http://www.bmj.com/content/341/bmj.c5204?sso=
http://lifeinthefastlane.com/subarachnoid-haemorrhage/
http://radiopaedia.org/articles/subarachnoid-haemorrhage
http://radiopaedia.org/articles/subarachnoid-haemorrhage
Sunday, 20 April 2014
Temporal Arteritis
Temporal arteritis is a rare cause of a headache but one that I always worry about missing. I remember as an FY2 in GP land, my tutor running through an examination on how to exclude serious causes of a headache. She palpated the temporal arteries - and now, I always do too!
AnatomyThinking about the anatomy of the carotid arteries is a good start to understanding the pathophysiology of temporal arteritis. For some reason, although any artery could be affected, the carotid arteries are much more frequently affected.


The superficial temporal artery is a branch of the external carotid artery. To test yourself on anatomy, I'd recommend the lumen website. If you look at the anatomical pictures, the vessel I used to think about as the temporal artery is not - and the temporal artery is a lot higher and more posterior than I realise.
To remember the branches:
"Some Anatomists Like Fornication, Others Prefer S & M"
S - Superior Thyroid Artery
A - Ascending Pharyngeal Artery
L - Lingual Artery
F - Facial Artery
O - Occipital Artery
P - Posterior Auricular Artery
S - Superficial Temporal Artery
M - Maxillary Artery
PathophysiologyOnce again, the Calgary Guide summarises everything you need to know. It is important to remember that the acute phase reaction can cause both a fever, and raised inflammatory markers so a careful history and examination is needed - you're unlikely to be treating meningitis!
Histology shows intimal proliferation with giant cells, evidence of elastic lamina damage and periarterial lymphocytic infiltration. Because temporal arteritis causes skip lesions, biopsies need to be taken at more than one place.
About 50% of patients with giant cell arteritis also have polymyalgia rheumatica and 15% to 20% of patients with polymyalgia rheumatica have evidence of giant cell arteritis on biopsy
Clinical Presentation
Again, the Calgary Guide covers everything! Headache and scalp tenderness is the presenting symptom most people comment on, but don't forget jaw claudication and stroke or TIA like symptoms.
The American College of Rheumatology has criteria for diagnosing giant cell arteritis. These were written a long time ago in 1990, and as far as I can tell, haven't been updated! Diagnosis can be made if the patient has at least three of these criteria. This gives a sensitivity of 93.5% and a specificity of 91.2%.
1. Age at disease onset >=50 years
2. New headache
3. Temporal artery abnormality
Temporal artery tenderness to palpation or decreased pulsation, unrelated to arteriosclerosis of cervical arteries. I'm not sure how you prove it's unrelated to arteriosclerosis!
4. Elevated erythrocyte sedimentation rate
Erythrocyte sedimentation rate >=50 mm/hour. This happens in 95% of patients. CRP is often used instead, and one study suggests it is a more sensitive marker than ESR.
5. Abnormal artery biopsy.
The temporal artery biopsy may be normal in 42% to 61% of the patients.
Imaging
A normal colour duplex ultrasound of the temporal artery makes giant cell arteritis unlikely with a negative predictive value of greater than 95%.
Treatment
- Prednisolone 40 mg daily
(If sight affected 60mg if just pmr 15mg)
- Temporal artery biopsy within two weeks.
- Reduce the dose after one to two months of treatment.
- 30% to 50% of patients can stop taking steroids after two years
- Remember bone protection. Bisphosphonates, calcium and vitamin d.
- PPI if on NSAID too - not if just on prednisolone.
- Rheumatology referral, especially if frequent relapses and patients are unable to reduce their dose of prednisolone to an acceptable level.
Prognosis
The symptoms of GCA should improve in one to two weeks. Symptoms of polymyalgia improve in 48 to 72 hours.
Other Similar Diseases
Takayasu's arteritis affects young women and causes:
Absent pulses in the arms
Neck bruits
Transient ischaemic attacks
Visual symptoms.
Polyarteritis nodosa causes:
Muscle pains
"Abdominal angina"
Livedo reticularis
Anaemia
Leucocytosis
Proteinuria
Raised ESR.
Polymyositis is most common in middle-aged women. It causes:
Pain and weakness in proximal muscles
A very elevated creatinine kinase.
Many patients with polymyositis have antinuclear antibodies.
References
http://learning.bmj.com/learning/module-intro/giant-cell-arteritis-diagnosis-treatment.html?moduleId=5001096&searchTerm=%E2%80%9Ctemporal%20arteritis%E2%80%9D&page=1&locale=en_GB
http://www.ncbi.nlm.nih.gov/pubmed/22119103
http://learning.bmj.com/learning/module-intro/.html?moduleId=10037282&searchTerm=%E2%80%9Ctemporal%20arteritis%E2%80%9D&page=1&locale=en_GB
http://bestbets.org/bets/bet.php?id=708http://ard.bmj.com/content/58/6/335.full
http://www.rheumatology.org/ACR/practice/clinical/classification/tcatree.asp
http://www.rheumatology.org/ACR/practice/clinical/classification/tca.asp
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Giant%20Cell%20%28Temporal%29%20Arteritis%20-%20Pathogenesis%20and%20investigations.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Giant%20Cell%20%28Temporal%29%20Arteritis%20-%20Clinical%20findings%20and%20Complications.jpg
AnatomyThinking about the anatomy of the carotid arteries is a good start to understanding the pathophysiology of temporal arteritis. For some reason, although any artery could be affected, the carotid arteries are much more frequently affected.

The superficial temporal artery is a branch of the external carotid artery. To test yourself on anatomy, I'd recommend the lumen website. If you look at the anatomical pictures, the vessel I used to think about as the temporal artery is not - and the temporal artery is a lot higher and more posterior than I realise.
To remember the branches:
"Some Anatomists Like Fornication, Others Prefer S & M"
S - Superior Thyroid Artery
A - Ascending Pharyngeal Artery
L - Lingual Artery
F - Facial Artery
O - Occipital Artery
P - Posterior Auricular Artery
S - Superficial Temporal Artery
M - Maxillary Artery
PathophysiologyOnce again, the Calgary Guide summarises everything you need to know. It is important to remember that the acute phase reaction can cause both a fever, and raised inflammatory markers so a careful history and examination is needed - you're unlikely to be treating meningitis!
Histology shows intimal proliferation with giant cells, evidence of elastic lamina damage and periarterial lymphocytic infiltration. Because temporal arteritis causes skip lesions, biopsies need to be taken at more than one place.
About 50% of patients with giant cell arteritis also have polymyalgia rheumatica and 15% to 20% of patients with polymyalgia rheumatica have evidence of giant cell arteritis on biopsy
Clinical Presentation
Again, the Calgary Guide covers everything! Headache and scalp tenderness is the presenting symptom most people comment on, but don't forget jaw claudication and stroke or TIA like symptoms.
The American College of Rheumatology has criteria for diagnosing giant cell arteritis. These were written a long time ago in 1990, and as far as I can tell, haven't been updated! Diagnosis can be made if the patient has at least three of these criteria. This gives a sensitivity of 93.5% and a specificity of 91.2%.
1. Age at disease onset >=50 years
2. New headache
3. Temporal artery abnormality
Temporal artery tenderness to palpation or decreased pulsation, unrelated to arteriosclerosis of cervical arteries. I'm not sure how you prove it's unrelated to arteriosclerosis!
4. Elevated erythrocyte sedimentation rate
Erythrocyte sedimentation rate >=50 mm/hour. This happens in 95% of patients. CRP is often used instead, and one study suggests it is a more sensitive marker than ESR.
5. Abnormal artery biopsy.
The temporal artery biopsy may be normal in 42% to 61% of the patients.
Imaging
A normal colour duplex ultrasound of the temporal artery makes giant cell arteritis unlikely with a negative predictive value of greater than 95%.
Treatment
- Prednisolone 40 mg daily
(If sight affected 60mg if just pmr 15mg)
- Temporal artery biopsy within two weeks.
- Reduce the dose after one to two months of treatment.
- 30% to 50% of patients can stop taking steroids after two years
- Remember bone protection. Bisphosphonates, calcium and vitamin d.
- PPI if on NSAID too - not if just on prednisolone.
- Rheumatology referral, especially if frequent relapses and patients are unable to reduce their dose of prednisolone to an acceptable level.
Prognosis
The symptoms of GCA should improve in one to two weeks. Symptoms of polymyalgia improve in 48 to 72 hours.
MT “@JAMA_current: #Headache, pain chewing, & tenderness💡 #TemporalArteritis ⬆️ http://t.co/Lw352M0NVx #RatlClinExam pic.twitter.com/P5FXudvP9H”
— Ixekizumab (@Brodalumab) April 20, 20145-10% of central retinal artery occlusions are associated with temporal aka giant cell arteritis #themoyouknow #usmle
— JGu (@absolutjag9) April 19, 2014#Headache, jaw claudication, & scalp tenderness? #TemporalArteritis more likely http://t.co/vv9IB4WVE3 #RatlClinExam pic.twitter.com/rZfIjfVAD5
— JAMA (@JAMA_current) April 19, 2014Other Similar Diseases
Takayasu's arteritis affects young women and causes:
Absent pulses in the arms
Neck bruits
Transient ischaemic attacks
Visual symptoms.
Polyarteritis nodosa causes:
Muscle pains
"Abdominal angina"
Livedo reticularis
Anaemia
Leucocytosis
Proteinuria
Raised ESR.
Polymyositis is most common in middle-aged women. It causes:
Pain and weakness in proximal muscles
A very elevated creatinine kinase.
Many patients with polymyositis have antinuclear antibodies.
References
http://learning.bmj.com/learning/module-intro/giant-cell-arteritis-diagnosis-treatment.html?moduleId=5001096&searchTerm=%E2%80%9Ctemporal%20arteritis%E2%80%9D&page=1&locale=en_GB
http://www.ncbi.nlm.nih.gov/pubmed/22119103
http://learning.bmj.com/learning/module-intro/.html?moduleId=10037282&searchTerm=%E2%80%9Ctemporal%20arteritis%E2%80%9D&page=1&locale=en_GB
http://bestbets.org/bets/bet.php?id=708http://ard.bmj.com/content/58/6/335.full
http://www.rheumatology.org/ACR/practice/clinical/classification/tcatree.asp
http://www.rheumatology.org/ACR/practice/clinical/classification/tca.asp
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Giant%20Cell%20%28Temporal%29%20Arteritis%20-%20Pathogenesis%20and%20investigations.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Giant%20Cell%20%28Temporal%29%20Arteritis%20-%20Clinical%20findings%20and%20Complications.jpg
Thursday, 17 April 2014
Migraines
Pathophysiology

I think this picture from the amazing Calgary guide summarises everything very well.
Basically, something starts it off - we don't know why. Everything gets sensitised, and the patient has lots of pain. The pain fibres in the walls of intercerebral blood vessels are part of the trigemial nerve, which also supplies sensation to the face. This is why referred pain is common.
Epidemiology and Triggers
Migraine is three times more prevalent in women (about 18% of the population) than in men (about 6%).

Food includes MSG, tyramine - containing foods and nitrate containing foods (and skipped meals!)
Menstruation is a migraine trigger in 10% of women with migraine. This is often overestimated by the patient: true menstrual migraine can be diagnosed only after examining a few months of the headache and menstrual diary. The OCP may help, but the helpful effect is lost during the pill free week.
There is an increased risk of fatal ischaemic stroke in people with migraine with aura, increased in people using combined hormonal contraception.morrhagic stroke.
Clinical Features
To officially diagnose migraines, the following criteria must be met:
The headache should have two or more of the following characteristics:
Unilateral location
Pulsating quality
Moderate to severe pain intensity
Aggravated by or causing avoidance of routine physical activity.
The headache should be accompanied by one or more of:
Nausea
Vomiting
Photophobia
Phonophobia.
The headache should not be attributable to another disorder and there should be no red flags (abnormal neurology, systemic symptoms such as fevers, chills, and weight loss, rapid increase in headache frequency, orthostatic worsening of symptoms, exertional worsening of symptoms, new onset, thunderclap headaches (very severe headache that reaches maximum intensity in <1 min), with existing risk factors for a secondary headache (such as cancer or hypercoagulable state) or overuse of headache abortive drugs.
This is nicely summarised with this mneumonic:
When does a "normal headache" become a migraine? You can have migraine with or without aura. Most of my headaches could be officially diagnosed as migraine. I call them a migraine if I HAVE to go to bed, and a headache if I struggle on with pain killers. But officially... Officially migraine causes bed rest or severe impairment in more than half of people.
Other useful pointers to a diagnosis of migraine include:
family history of headache/ migraine
motion sickness or cyclical vomiting as a child
delayed headache following alcohol, or "unfair" tendency to hangovers
typical migraine triggers, for example sleep disturbance, missing meals, relaxation, pre- or perimenstrual timing, cheese, wine, chocolate, citrus, etc
Typical aura symptoms include visual, sensory and speech symptoms. Visual symptoms are most common, and include flickering lights, spots or lines, or loss of vision (blind spots or scotoma). An aura typically lasts for <60 minutes, and usually precedes or sometimes accompanies the headache. Around a third of migraine sufferers report the experience of aura symptoms. Only just over half of migraine sufferers who experience aura experience it with every attack. Most aura symptoms last between 30 minutes and one hour and occur before the onset of pain.
Chronic migraine is properly defined as >15 days of headache per month, with >eight days being migraine, for at least three months. The definition excludes people who overuse medication
Treatment
Consider rectal treatment if IV inappropriate or for home. Do NOT use opiates!
Naproxen: NNT of 11.
Aspirin: 1000mg
Ibuprofen is more effective than paracetamol at pain relief for migraine attacks in children
Chlorpromazine: IV + NaCl
Prochlorperazine: 10mg IV + NaCl is better than metoclopramide
Metoclopramide: Conflicting evidence
Haloperidol: 2.5 mg of haloperidol as a substitute (the literature on this is scarce, and some of it is old).
Triptans: More effective if taken in the prodromal window. They block the stimulation of the trigeminal ganglion and preventing the sensation of pain. The triptans are selective 5-hydroxytryptamine (5HT) receptor agonists, with high affinity for the 5HT1B and 5HT1D receptors. 5HT1B receptors are on smooth muscle cells of blood vessels and cause vasoconstriction when stimulated.
Around 1-7% of participants in clinical trials (without cardiovascular disease) experience “triptan sensations”—a burning, tingling, or tightness in the face, neck, limbs, or chest—which is not associated with electrocardiographic or enzymatic evidence of myocardial ischaemia.
Triptans are not recommended for use in pregnancy or in the presence of coronary heart disease, as there are also receptors in the coronary arteries.
Propofol: 20-30mg every 3 - 5minutes reduces pain quickly and effectively. I don't think it'd ever be in my top million treatments!
Dexamethasone: 26% relative reduction in headache recurrence (number needed to treat=9) in 72 hours.
Prophylaxis
Pharmacological prophylaxis is recommended in those who:
- Have frequent, high impact migraine attacks (>4 per month)
- Are not treated satisfactorily with appropriate acute medications
- Have concomitant conditions that do not allow the use of acute medications (for example, a migraine variant)
- Are overusing acute medications, or have chronic primary headache, or both
- Advice on behavioural and physical therapies, including acupuncture, relaxation, biofeedback, stress reduction, cervical manipulation, massage, exercise and avoiding migraine triggers. Change in sleeping times at weekends and irregular shift work may usefully be avoided, as is the abrupt let-down from stress.
- Feverfew, magnesium, and vitamin B2
Propanolol, topiramate and acupuncture should be considered.
References:
http://jnnp.bmj.com/content/early/2012/07/23/jnnp-2012-302487
http://circ.ahajournals.org/content/118/14/1405.full
http://emupdates.com/2009/11/23/migraine-criteria-for-diagnosis/
http://socmob.org/2013/11/propofol-migraine-part-2/
http://bestbets.org/bets/bet.php?id=545
http://bestbets.org/bets/bet.php?id=88
http://bestbets.org/bets/bet.php?id=504http://bestbets.org/bets/bet.php?id=787
http://bestbets.org/bets/bet.php?id=1036http://bestbets.org/bets/bet.php?id=2454
http://bestbets.org/bets/bet.php?id=2333
http://bestbets.org/bets/bet.php?id=2045
http://bestbets.org/bets/bet.php?id=2074http://bestbets.org/bets/bet.php?id=2458
http://academiclifeinem.com/on-the-horizon-propofol-for-migraines/
http://annals.org/article.aspx?articleid=715803http://empharmd.blogspot.co.uk/2013/05/milking-it-propofol-for-migraine.html
http://jnnp.bmj.com/content/72/suppl_2/ii10.full
http://learning.bmj.com/learning/module-intro/preventive-%CE%B2-blocker-migraine-optimised-acute-migraine.html?moduleId=10017044&searchTerm=%E2%80%9Cmigraine%E2%80%9D&page=1&locale=en_GB
http://www.bmj.com/content/348/bmj.g1416.pdf%2Bhtml
http://www.bmj.com/content/347/bmj.f6952.pdf%2Bhtml
http://bestbets.org/bets/bet.php?id=1416
http://www.enlightenme.org/node/2331
http://learning.bmj.com/learning/module-intro/migraine-diagnosis-prevention.html?moduleId=5003207&searchTerm=%E2%80%9Cmigraine%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/migraine-patient-experience-pathology-therapies.html?moduleId=10021852&searchTerm=%E2%80%9Cmigraine%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/migraine-haemorrhagic-stroke-women.html?moduleId=10016760&searchTerm=%E2%80%9Cmigraine%E2%80%9D&page=1&locale=en_GB
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Migraines%20and%20Auras%20Pathogenesis%20and%20Clinical%20Findings.jpg
Tension Headache
Re @embasic
The proper dose of opioids for acute headache is 0.0 mg/kg
#foamed
— Mike Abernethy (@FLTDOC1) April 3, 2014
Tension Headache and Medication Overuse headache are very similar in my head (the former sometimes literally), so I'm going to cover both of them together!Tension Headache
Tension headache can be episodic or chronic. It is normally described as a featureless headache. It can cause daily or very frequent headaches, lasting minutes to days.
- Symptoms begin before the age of 10 years in 15% of people with chronic tension-type headache.
- It affects 4.1% of the population
- 65% of cases are women
It is thought to be triggered at least partially by stress.
The 2004 International Headache Society criteria for chronic tension-type headache are:
- Headaches on 15 or more days a month (180 days/year) for at least three months
- Pain that is bilateral, pressing, or tightening in quality and non-pulsating, of mild or moderate intensity, which does not worsen with routine physical activity such as walking or climbing stairs
- Presence of no more than one additional clinical feature (mild nausea, photophobia, or phonophobia) and without moderate/severe nausea or vomiting.
- Causes of normal headache --> chronic daily headache:
Interesting review of tension headache therapeutics in ED http://t.co/74XEv6lqMG #FOAMed #FOAM4GP
— Casey Parker (@broomedocs) March 15, 2014
Treatment
- Prevention is better than cure
- Amitriptyline or mirtazapine are both helpful
- CBT
Medication Overuse Headache
Medication overuse headache is difficult to diagnose, as the type of headache that develops varies eg patients with underlying migraine report migraine-like daily headache.
It is caused by tolerance, and withdrawal.
They normally use large quantities of medication (eg 35 doses/ week; six different drugs). Opiods and barbiturates are more likely to cause it.
It is the frequence rather than the absolute quantity that is important. Caffeine is thought to make you more susceptible.
- Prevalence around 1% of adults and 0.5% of adolescents (aged 13–18 years)
- Most prevalent in those aged around 40–50 years and affects about three times more women than men.
Symptoms improve 1- 6 months after withdrawal of medication. Simply recognising medication overuse and advising patients about its bad effects can be enough to significantly reduce the problem- in one study after identification of the problem, 76% no longer overused medication, and 42% no longer had chronic headache. The rate of relapse is high (between one-third and one-half of patients in specialist headache clinics), being more likely with opiates and simple analgesics than triptans.
References
http://dtb.bmj.com/content/48/1/2.abstract
http://learning.bmj.com/learning/module-intro/chronic-tension-headache.html?moduleId=10007571&searchTerm=%E2%80%9Ctension%E2%80%9D&page=1&locale=en_GB
http://bestpractice.bmj.com/best-practice/monograph/12.html
http://www.bmj.com/content/336/7635/88?variant=pdf&sso=
http://emupdates.com/2009/01/03/664-features-of-tension-headache-causes-of-subarachnoid-hemorrhage-what-of-the-population-has-a-berry-aneurysm-diseases-associated-with-berry-aneurysm/ http://www.bmj.com/content/340/bmj.c1305
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1517
Friday, 11 April 2014
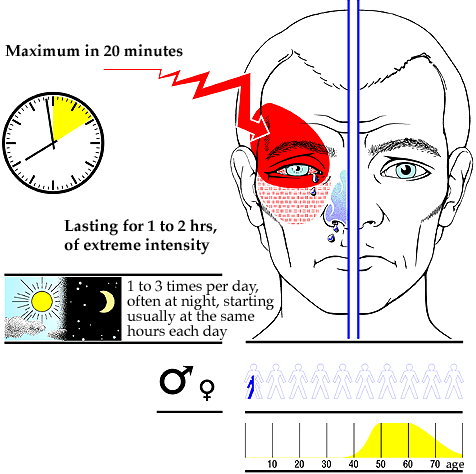
Cluster Headaches
Cluster headaches are severe unilateral headaches. They used to be called migranous neuralgia. They are short lasting and are accompanied by autonomic symptoms. Less than 1% of patients have cluster headache, and it affects men more than women (3- 6 times more), and young people (in their 30s) rather than old people. 85% of patients smoke. They present similarly in men and women, but women tend to have more migrainous type symptoms. Alcohol, nitroglycerine, exercise, and elevated environmental temperature are recognized precipitants of acute cluster attacks.
Symptoms
- Short bouts of pain, lasting weeks or months
- Bouts may occur up to eight times a day
- Follow a circadian rhythm, with a 24hour cycle
- One sided in the orbital, supraorbital or temporal regions
- Associated with autonomic symptoms (ptosis, miosis, eye watering, bloodshot eye, runny nose, blocked nose).
- Autonomic symptoms occur on the same side as the pain
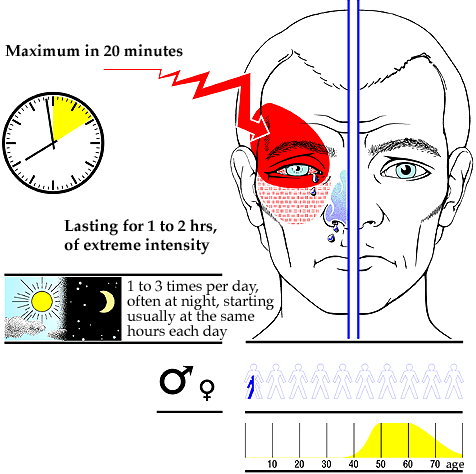

Official Diagnosis
A diagnosis of cluster headache is supported by at least five attacks that fulfil the following criteria:
Severe pain on one side in the orbital, supraorbital, or temporal region which lasts 15 to 180 minutes if left untreated.
At least one of the following on the same side:
Bloodshot or watery eye
Blocked or runny nose
Eyelid oedema
Forehead and facial sweating
Miosis or ptosis, or both
A sense of restlessness or agitation
Attacks that occur every other day at a frequency of up to eight per day
Other causes have been excluded.
Migraine vs Cluster Headache
Alcohol induces cluster headache quickly, migraines some hours after.
Treatment
To manage patients with cluster headache you should treat the acute attack and consider prophylaxis against further attacks
Oxygen
- 100% via non re-breath mask for at least 20 minutes
- 60% of patients respond to oxygen therapy
- More beneficial at the onset of symptoms
Sumatriptan
- 6mg sc sumatriptan relieves pain in 20minutes in 75% of patients
- Oral triptans are too slow
- Triptans contraindicated with cardiovascular, cerebrovascular disease and untreated arterial hypertension. Do NOT use with MAOIs or ergotamines.
- Side effects include chest pain and distal paraesthesiae.
Ergotamines
Oral ergotamine has been used to treat cluster headache for more than 50 years, but there is little evidence available to support its effectiveness.
Lidocaine
Applying lidocaine nasally is effective in about one third of patients. The suggested dosage is 1 ml with a concentration of 4-10%, given on the same side as the pain. The patient should lie back with their head turned to the affected side after application. Most of these studies are small, and the effect is unlikely to be clinically beneficial.
Steroids
Up to 80% of patients with cluster headache respond to steroids. Start with 60-100 mg of prednisolone once a day for at least five days. After this you should try to decrease the dosage by 10 mg every day.
Third Line Treatment
Pizotifen, valproic acid, topiramate and capsaicin. Prevent with verapamil or lithium.
Follow Up
It is recommended that patients attending with cluster headaches should be followed up in neurology outpatients for consideration of further imaging as there is a link with pituitary adenoma.
Paroxysmal hemicrania
Paroxysmal hemicrania is rare. It is similar to cluster headaches but patients have shorter, more frequent attacks. They have a good response to indomethacin. This is one of the diagnostic criteria. Within three to seven days of starting indomethacin at an adequate dosage the attacks disappear. The usual dose is 50 mg three times per day. It is worth trying a trial of indomethacin even if the headache is not typical of paroxysmal hemicrania; if patients are going to respond, they will do so quickly.
http://www.enlightenme.org/learning-zone/doc-my-head-hurts
http://www.bmj.com/content/344/bmj.e2407
http://jnnp.bmj.com/content/70/5/613.full
http://www.pn.bmj.com/content/1/1/42.full.pdf
http://www.bmj.com/content/344/bmj.e2407.pdf%2Bhtml
http://n3.learning.bmj.com/learning/modules/flow/JIT.html?execution=e1s1&_flowId=JIT&moduleId=5004479&status=LIVE&locale=en_GB&action=start&sessionTimeoutInMin=90
http://cks.nice.org.uk/headache-cluster
http://publications.nice.org.uk/headaches-cg150
http://www.sign.ac.uk/guidelines/fulltext/107/index.html
Symptoms
- Short bouts of pain, lasting weeks or months
- Bouts may occur up to eight times a day
- Follow a circadian rhythm, with a 24hour cycle
- One sided in the orbital, supraorbital or temporal regions
- Associated with autonomic symptoms (ptosis, miosis, eye watering, bloodshot eye, runny nose, blocked nose).
- Autonomic symptoms occur on the same side as the pain

Official Diagnosis
A diagnosis of cluster headache is supported by at least five attacks that fulfil the following criteria:
Severe pain on one side in the orbital, supraorbital, or temporal region which lasts 15 to 180 minutes if left untreated.
At least one of the following on the same side:
Bloodshot or watery eye
Blocked or runny nose
Eyelid oedema
Forehead and facial sweating
Miosis or ptosis, or both
A sense of restlessness or agitation
Attacks that occur every other day at a frequency of up to eight per day
Other causes have been excluded.
Migraine vs Cluster Headache
Alcohol induces cluster headache quickly, migraines some hours after.
Treatment
To manage patients with cluster headache you should treat the acute attack and consider prophylaxis against further attacks
Oxygen
- 100% via non re-breath mask for at least 20 minutes
- 60% of patients respond to oxygen therapy
- More beneficial at the onset of symptoms
Sumatriptan
- 6mg sc sumatriptan relieves pain in 20minutes in 75% of patients
- Oral triptans are too slow
- Triptans contraindicated with cardiovascular, cerebrovascular disease and untreated arterial hypertension. Do NOT use with MAOIs or ergotamines.
- Side effects include chest pain and distal paraesthesiae.
Ergotamines
Oral ergotamine has been used to treat cluster headache for more than 50 years, but there is little evidence available to support its effectiveness.
Lidocaine
Applying lidocaine nasally is effective in about one third of patients. The suggested dosage is 1 ml with a concentration of 4-10%, given on the same side as the pain. The patient should lie back with their head turned to the affected side after application. Most of these studies are small, and the effect is unlikely to be clinically beneficial.
Steroids
Up to 80% of patients with cluster headache respond to steroids. Start with 60-100 mg of prednisolone once a day for at least five days. After this you should try to decrease the dosage by 10 mg every day.
Third Line Treatment
Pizotifen, valproic acid, topiramate and capsaicin. Prevent with verapamil or lithium.
Follow Up
It is recommended that patients attending with cluster headaches should be followed up in neurology outpatients for consideration of further imaging as there is a link with pituitary adenoma.
Paroxysmal hemicrania
Paroxysmal hemicrania is rare. It is similar to cluster headaches but patients have shorter, more frequent attacks. They have a good response to indomethacin. This is one of the diagnostic criteria. Within three to seven days of starting indomethacin at an adequate dosage the attacks disappear. The usual dose is 50 mg three times per day. It is worth trying a trial of indomethacin even if the headache is not typical of paroxysmal hemicrania; if patients are going to respond, they will do so quickly.
http://www.enlightenme.org/learning-zone/doc-my-head-hurts
http://www.bmj.com/content/344/bmj.e2407
http://jnnp.bmj.com/content/70/5/613.full
http://www.pn.bmj.com/content/1/1/42.full.pdf
http://www.bmj.com/content/344/bmj.e2407.pdf%2Bhtml
http://n3.learning.bmj.com/learning/modules/flow/JIT.html?execution=e1s1&_flowId=JIT&moduleId=5004479&status=LIVE&locale=en_GB&action=start&sessionTimeoutInMin=90
http://cks.nice.org.uk/headache-cluster
http://publications.nice.org.uk/headaches-cg150
http://www.sign.ac.uk/guidelines/fulltext/107/index.html
Sunday, 6 April 2014
Practical Procedures: Cardioversion and Pacing
I very much didn't like doing cardioversions, or pacing until I actually did them! I still find it difficult to remember the numbers, so I've got myself a special memory card - it's duplicated information elsewhere, but better too many times than not enough.
Syncope
Syncope is common, and difficult to investigate because by definition, the patient has recovered from the event! It is summarised here. There are five main causes to consider:
1. Neurocardiogenic or vasovagal (emotional, situational or orthostatic triggers)
2. Cardiac
3. Orthostatic
4. Neurological / psychiatric (5%). Neurological causes of syncope include basilar artery migraine, vestibular dysfunction and vertebrobasilar ischaemia. Psychiatric syncope is a recognised syndrome consisting of syncopal episodes found in anxiety, depression and conversion disorder that resolve with treatment of the psychiatric disorder.
5. Essential (no cause found -35-50%).
These will all be covered in turn, and separately. There are scoring systems used to help risk-stratify syncope (very important). I do like EM Basic's quick approach:
OESIL (Osservatorio Epidemiologico della Sincope nel Lazio) Score
The San Francisco Rule
The San Francisco rule identifies high risk patients based on the presence of the following factors:
The EGSYS (derived from patients enrolled in the Evaluation of Guidelines in SYncope Study 2 trial) Score
This specifically identified cardiac syncope with a score of 3 or
more being 99% sensitive and 65% specific for identifying cardiac
syncope (positive and negative predictive values 33% and 99%). Again, I've never seen this used in clinical practice.
Investigations
A completely normal ECG makes a cardiac cause of syncope other than transient arrhythmia unlikely.
Echocardiography should be performed in any patient with a cardiac murmur and to diagnose and quantify suspected heart failure. If aortic stenosis is suspected, echocardiography should be performed urgently.
Carotid sinus massage for 5 to 10 seconds with continuous ECG and blood pressure monitoring can be used to diagnose carotid sinus syndrome. It is considered positive if it produces a drop in systolic blood pressure of 50 mm Hg or a period of asystole of 3 seconds.
Ambulatory 24 hour ECG recording may be considered in patients with a high pre-test probability of arrhythmia.
Tilt table testing is not used much any more
Management
Think about all causes - 18% of patients with syncope in one study had more than one cause.
Driving - consider whether the patient should refrain from driving
Other guidelines can be found here.
1. Neurocardiogenic or vasovagal (emotional, situational or orthostatic triggers)
2. Cardiac
3. Orthostatic
4. Neurological / psychiatric (5%). Neurological causes of syncope include basilar artery migraine, vestibular dysfunction and vertebrobasilar ischaemia. Psychiatric syncope is a recognised syndrome consisting of syncopal episodes found in anxiety, depression and conversion disorder that resolve with treatment of the psychiatric disorder.
5. Essential (no cause found -35-50%).
These will all be covered in turn, and separately. There are scoring systems used to help risk-stratify syncope (very important). I do like EM Basic's quick approach:
Syncope + headache= subarachnoid or intracranial hemorrhage
Syncope + neuro deficit= stroke/TIA or intracranial bleed
Syncope + confusion= seizure
Syncope + chest pain= MI, PE, or aortic dissection
Syncope + back/abdominal pain in older patient= abdominal aortic aneurysm (AAA)
Syncope + positive HCG= ectopic pregnancy
Young with Syncope R/O:
Structural heart prob HOCM
Elect (brugada, prolonged QT, arrhythmia)
Hypoglycaemia
CNS insult
Abnormal Lytes
#FOAMed
— Meshal AlBassam (@meshal_albassam) March 16, 2014
OESIL (Osservatorio Epidemiologico della Sincope nel Lazio) Score
- age over 65 years;
- previous history of cardiovascular disease;
- syncope without prodrome and
- abnormal ECG
The San Francisco Rule
The San Francisco rule identifies high risk patients based on the presence of the following factors:
- History of congestive cardiac failure
- Haematocrit < 30%
- Abnormal ECG
- Complaint of shortness of breath
- Systolic Blood Pressure < 90 mm Hg
The EGSYS (derived from patients enrolled in the Evaluation of Guidelines in SYncope Study 2 trial) Score
| Predictor | Score |
| Palpitations preceding syncope | 4 |
| Syncope during effort | 3 |
| Heart disease/ abnormal ECG | 3 |
| Syncope while supine | 2 |
| Precipitating/ predisposing factors | -1 |
| Autonomic prodromes | -1 |
Investigations
A completely normal ECG makes a cardiac cause of syncope other than transient arrhythmia unlikely.
Echocardiography should be performed in any patient with a cardiac murmur and to diagnose and quantify suspected heart failure. If aortic stenosis is suspected, echocardiography should be performed urgently.
Carotid sinus massage for 5 to 10 seconds with continuous ECG and blood pressure monitoring can be used to diagnose carotid sinus syndrome. It is considered positive if it produces a drop in systolic blood pressure of 50 mm Hg or a period of asystole of 3 seconds.
Ambulatory 24 hour ECG recording may be considered in patients with a high pre-test probability of arrhythmia.
Tilt table testing is not used much any more
@drsuneet @SergioPinski @MGKatz036 To me, tilts worthless in eval of syncope. Not reproducible and high false pos/neg rates.
— Westby Fisher, MD (@doctorwes) April 6, 2014
Management
Think about all causes - 18% of patients with syncope in one study had more than one cause.
Driving - consider whether the patient should refrain from driving
Other guidelines can be found here.
Subscribe to:
Posts (Atom)
















