RUQ - Pouch of Rutherford-Morrison
- Start just anterior to the mid-axillary line, angled slightly backwards.
- Slide the probe towards the head to get a view of the diaphragm
- Look for pleural fluid - a jet black triange just above the diaphragm
- Ask the patient to take a deep breath if possible, particularly if rib shadows obscure the area of interest.
LUQ - Spleno-renal angle
- Posterior-axillary line at about the 6th to 9th intercostal space
- To get rid of rib shadows, and to get a better view of the spleen, slide the probe towarsd the hed and rotate it very slightly clockwise, producing an intercostal oblique view, so that the spleen (not the kidney) is seen.
Pelvic - Pouch of Douglas in females, rectovesical pouch in male
Fluid will collect here.
Place the probe on the pubic bone and note a bone shadow. Slide slightly towards the head to get a good longitudinal pelvic view.
Full bladder will be triangular in shape.
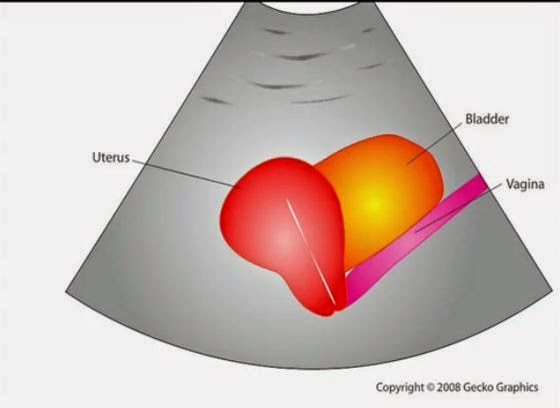
In a female, the body of the uterus sits in the intraperitoneal space just posterior to the bladder (Figure 19), so free fluid will be seen just posterior to the uterus. This space is often called the pouch of Douglas and sometimes just small amounts can be detected
Cardiac
Subxiphoid view - probe laid almost flat and angled towards the head. Apply probe pressure to indent the epigastrium
Pitfalls
Perinephric fat, especially in obese patients, may be misinterpreted as intraperitoneal free fluid. Consider comparison views between each kidney.
Free fluid isn’t always blood; consider ascites, fluid related to a ruptured ovarian cyst, ruptured bladder or peritoneal dialysis.
90% sensitive and 99% specific for traumatic haemoperitoneum
References
Emergency Ultrasound Made Easy
http://www.trauma.org/index.php/main/article/214/
http://www.sonoguide.com/FAST.html
CEM Website