Asthma is really common and affects lots of people. It also causes lots of unnecessary deaths, and a lot of hospital attendances from asthma attacks. The 2014 asthma guidelines replace the word "exacerbation" with "attack" as it's easier to understand.
References for this summary will be at the end of part two.
Physiology


Asthma is defined as a chronic airway inflammatory disorder with airway hyper-responsiveness.
Asthma is an obstructive lung condition, caused essentially by an allergic reaction to a trigger. Like most reactions, there is exposure that sensitizes the helper T cells, then IgE is produced, mast cells - and then you get the response on the second and subsequent exposure. The release of histamines and leukotrienes causes vasodilation, increased mucus secretion and bronchial smooth muscles contraction. The reaction also causes eosinophils to migrate into the airways, eyes and nose causing conjunctivitis, rhinitis and bronchiole constriction.
Clinical Features

The Calgary Guide has a nice summary here. There's no thing that says with 100% certainty that this is asthma.
These features increase the probability of asthma:
- >1 of wheeze, cough, difficulty breathing, chest tightness
- particularly if the symptoms:
are worse at night/early morning
occur in response to exercise, allergen exposure or cold air
are triggered by aspirin or beta-blockers
occur in the absence of a cold
- Personal or family history of atopic disorder or asthma
- Widespread wheeze on chest auscultation
- Otherwise unexplained low FEV1 or PEFR
- Otherwise unexplained peripheral blood eosinophilia
These features lower the probability of asthma:
- Symptoms with colds only
- Chronic productive cough without wheeze or breathlessness
- Dizzyness, light-headedness or paraesthesia peripherally
- Voice disturbance
- Cardiac disease
- Significant smoking history (>20 pack years)
- Repeated normal chest examination when symptomatic
- Repeatedly normal PEFR or spirometry when symptomatic
Grading Systems
The SIGN (and British Thoracic Society) guidelines use clinical symptoms to grade the severity of an attack in adults and children. The NICE guidelines appear to be based on the SIGN guidelines.
Systolic paradox (pulsus paradoxus), an historical marker of severity of asthma, is unhelpful and wastes valuable time so has been removed from the guidelines.
Features of patients at high risk of a life-threatening asthma attack:
Using a short-acting beta agonist inhaler more than once every four hours
Using more than one short-acting bronchodilator inhaler per month
Fewer than 12 prescriptions for preventer medication in the past year
Concurrent mental health problems
Investigations
Normally a clinical diagnosis, but if the patient has an intermediate probability of asthma, investigations can help. The Calgary guide has a summary.
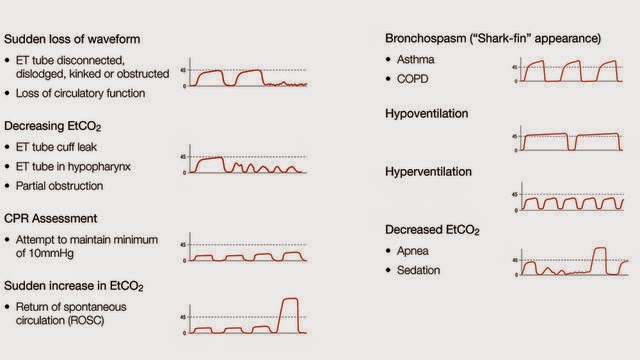
Capnography:
Wave form capnography should be used in acute exacerbations. Asthmatics get a "shark's fin" appearance because of the broncho-constriction.
Spirometry:
Spirometry shows reversibility and FEV1/FVC <0.7:
A decrease in FEV1 of > 15% after six minutes of exercise, or
An increase in FEV1 of > 15% after a two week trial of oral steroids (30 mg prednisolone once
daily), or
An increase in FEV1 of > 15% following therapy with a short acting beta 2 agonist
You can calculate the percentage change in FEV1 by:
Subtract the pre-bronchodilator FEV1 from the post-bronchodilator FEV1
Divide this by the pre-bronchodilator FEV1
Multiply by 100.
Peak Flow
60l/min. increase in PEFR) in response to either of the following strongly suggests underlying asthma:
400 mcg inhaled salbutamol
6-week trial of steroid inhaler (beclometasone 200 mcg bd or equivalent)
CXR
- Normal in up to 75% of patients
- pulmonary hyperinflation
- bronchial wall thickening - peribronchial cuffing
(non specific finding but may be present in ~48% of cases with asthma)
- pulmonary oedema due to asthma
CT
To look for complicated associated conditions such as allergic bronchopulmonary aspergillosis and not to directly diagnose asthma.
Non specific:
- bronchial wall thickening
- expiratory air trapping
- inspiratory decreased lung attenuation
- small centrilobular opacifities
- bronchial luminal narrowing - reduced
- bronchoarterial-diameter ratio
- sub segmental bronchiectasis - may be present in ~28-62% of asthmatics
Mimics
• Churg-Strauss
Look for signs and symptoms of systemic vasculitis, such as fever, weight loss, fatigue, and malaise, Be suspicious if there is a persistent eosinophilia, positive ANCA, and multiorgan involvement.
• COPD
• Anaphylaxis
4% of asthma admissions to PICU almost certainly had anaphylaxis rather than asthma - so make sure you consider it.
• Rhinitis
Management of chronic rhinosinusitis improves asthma control.
• Gastro-oesophageal reflux
Consider a three month trial of PPIs, as investigations to formally diagnose this are very invasive.
• Inhaled foreign body
• Airway stenosis
• Bronchiectasis
• Sarcoidosis
• Lung cancer
• Obliterative bronchioloitis
• Congestive cardiac
failure
• Pulmonary embolus
• Pulmonary fibrosis
• Hyperventilation syndrome
• Chronic cough syndrome
• Vocal cord dysfunction
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.





Thank heavens this Informative article is fascinating and clear. Others I've perused caused me to feel like I required a degree to translate them. Much obliged to you. For more information visit here Lauq Katan
ReplyDeleteSo easy to understand. Bless you
ReplyDelete