GPs should be able to manage most asthma. The following points may be beneficial:
Steroids and "New" Drugs
Relvar Ellipta (GSK) is a dry powder inhaler that contains a corticosteroid (fluticasone furoate) and a long-acting beta2 agonist (vilanterol trifenatate). It is licensed for once-daily use as maintenance therapy for COPD and asthma.
Flixotide Evohaler is only available for the over 4s and Budesonide Easihaler only for those over 6. Seretide (fluticasone and serevent) is only for use in over 4s and Symbicort (budesonide and formoterol) only for the over 6s.
Methotrexate at low doses retains anti-inflammatory properties with little toxicity. In chronic severe asthma a number of mixed results have been reported with oral methotrexate.
Clinical issues
General questions, such as “how is your asthma today?” yield a non-specific answer; “I am ok”. Using closed questions, such as “do you use your blue inhaler every day?”, is likely to yield more useful information.
Education is a process and not a single event.
No patient should leave hospital without a written personalised asthma action plan.
Education should include personalised discussion of issues such as trigger avoidance and achieving a smoke-free environment to support people and their families living with asthma.
Brief simple education linked to patient goals is most likely to be acceptable to patients.
Do not recommend house dust mite avoidance to prevention asthma, or pet avoidance.
Treatment of reflux has no benefit in asthma control, although it does reduce dry cough.
Spacers
Single actuations of the metered dose inhaler into the spacer, each followed by inhalation.
Minimal delay between pMDI actuation and inhalation.
Tidal breathing is as effective as single breaths.
Spacers should be cleaned monthly rather than weekly as per manufacturer’s recommendations or performance is adversely affected. They should be washed in detergent and allowed to dry in air. The mouthpiece should be wiped clean of detergent before use.
Plastic spacers should be replaced at least every 12 months
References
http://bestbets.org/bets/bet.php?id=1768
Critical Care and Resuscitation 2005; 7: 119-127
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007524.pub3/abstract
http://www.enlightenme.org/knowledge-bank/cempaedia/asthma-adults
http://www.enlightenme.org/the-curriculum-zone/node/2734
http://www.enlightenme.org/knowledge-bank/journal-scan/3mg-trial-randomised-trial-intravenous-or-nebulised-magnesium-sulphate-v
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002308.pub2/abstract
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002178/abstract
http://www.enlightenme.org/knowledge-bank/cem-ctr/acute-asthma-does-addition-magnesium-sulphate-have-clinically-significant-eff
http://www.enlightenme.org/learning-zone/acute-severe-wheeze-please
http://www.enlightenme.org/the-curriculum-zone/node/3771
http://www.enlightenme.org/knowledge-bank/cempaedia/breathlessness
http://www.aliem.com/lactic-acidosis-beta-agonist-therapy-asthma/
http://learning.bmj.com/learning/course-intro/asthmatic-patient.html?courseId=10046989&locale=en_GB = DONE
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002316.pub2/abstract
http://r1.emsworld.com/files/cygnus/image/EMSR/2011/AUG/640x360/pocketguide_patient_10342321.jpg
http://learning.bmj.com/learning/module-intro/quick-tips-asthma.html?moduleId=10050019&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/.html?moduleId=10051335&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/occupational-asthma-evidence-based-diagnosis-management.html?moduleId=6051298&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/modules/flow/MCQ.html?execution=e9s1&moduleId=10029655&status=LIVE&action=start&_flowId=MCQ&sessionTimeoutInMin=90&locale=en_GB
http://www.enlightenme.org/knowledge-bank/cempaedia/asthma-adults
http://www.enlightenme.org/the-curriculum-zone/node/2734
http://learning.bmj.com/learning/course-intro/asthmatic%20patient.html?courseId=10046989&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://dontforgetthebubbles.com/emergency-medicine-clinical-excellence-series-pem-2-allergy-anaphylaxis-children/
http://www.enlightenme.org/knowledge-bank/cem-ctr/acute-asthma-does-addition-magnesium-sulphate-have-clinically-significant-eff
http://www.enlightenme.org/knowledge-bank/journal-scan/3mg-trial-randomised-trial-intravenous-or-nebulised-magnesium-sulphate-v
http://www.enlightenme.org/learning-zone/acute-severe-wheeze-please
http://ccforum.com/content/6/1/30
http://radiopaedia.org/articles/peri-bronchial-cuffing-2
http://radiopaedia.org/articles/asthma-1
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Findings%20on%20Investigations.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Clinical%20Findings.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Pathogenesis.jpg
https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2014/
https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-quick-reference-guide-2014/
Tuesday, 11 November 2014
Asthma - treatment
Moderate Severity Asthma Exacerbation
- 4 puffs salbutamol via a spacer, followed by 2 puffs every 2 minutes up to a maximum of 10 puffs
- Nebulisers if no spacer available or if the patient can't use it effectively.
Severe Acute Asthma
Steroids: Inhaled corticosteroids in the acute attack can help reduce hospitalisation. Little evidence that on discharge they improve things. Corticosteroids within an hour also help
Nebulisers: Allow concurrent oxygen administration.
A nebuliser takes 15-30 minutes to fully administer the drug. Administering more than 10mg of salbutamol per hour is unlikely to improve effectiveness but may increase side effects, which include tremor and tachycardia. Special delivery systems can deliver “continuous” nebulisers at 10mg per hour but are not usually available in the ED.
There is no evidence that 5mg nebulisers are superior to 2.5mg nebulisers.
Inhaled salbutamol can cause a lactic acidosis, worsening respiratory symptoms.
Salbutamol: No superiority of IV salbutamol over acute asthma. Systemic salbutamol has metabolic effects that may worsen respiratory function in asthma.
May be helpful if drug not delivered effectively (patient pulling mask off/ poor air entry).
Adrenaline: Nebulised adrenaline has shown no superiority and is a less selective agonist.
Anticholinergic: advocated in cases which are severe, life-threatening, or poorly responsive to ß2 agonist therapy.
Magnesium: Nebulised MgSO4 has no role
Limited role for intravenous MgSO4
Aminophylline: 5mg/kg over 20minutes loading dose
0.6mg/kg/hour IV infusion
If the patient is on maintenance take a baseline theophylline/ aminophylline level before maintenance infusion.
Furosemide: A theoretical bronchodilator of research interest, not better than nebulised ß2 agonists.
Rapid Sequence Induction
Use at least a size 8.0 diameter
Ketamine --> 1-2mg/kg helps bronchodilate
Avoid atracurium
Disconnect circuit during CPR to allow chest to deflate
Bilateral thoracostomies.
Discharge
Steroids if PEFR initially <50% best or predicted.
Stop abruptly after five days as long as patient continues on inhaled steroids.
Careful discharging patients that present late in the evening or early hours of the morning since the airways are naturally at their narrowest at around 4am.
When any of the following features are present, admission may be appropriate:
Referral if:
Two courses of systemic corticosteroids in the past year
- 4 puffs salbutamol via a spacer, followed by 2 puffs every 2 minutes up to a maximum of 10 puffs
- Nebulisers if no spacer available or if the patient can't use it effectively.
Severe Acute Asthma
Early steroid administration in acute severe asthmatic exacerbations is associated with a reduced need for hospital admission.
Steroids: Inhaled corticosteroids in the acute attack can help reduce hospitalisation. Little evidence that on discharge they improve things. Corticosteroids within an hour also help
A nebuliser takes 15-30 minutes to fully administer the drug. Administering more than 10mg of salbutamol per hour is unlikely to improve effectiveness but may increase side effects, which include tremor and tachycardia. Special delivery systems can deliver “continuous” nebulisers at 10mg per hour but are not usually available in the ED.
There is no evidence that 5mg nebulisers are superior to 2.5mg nebulisers.
Inhaled salbutamol can cause a lactic acidosis, worsening respiratory symptoms.
Salbutamol: No superiority of IV salbutamol over acute asthma. Systemic salbutamol has metabolic effects that may worsen respiratory function in asthma.
May be helpful if drug not delivered effectively (patient pulling mask off/ poor air entry).
Adrenaline: Nebulised adrenaline has shown no superiority and is a less selective agonist.
Anticholinergic: advocated in cases which are severe, life-threatening, or poorly responsive to ß2 agonist therapy.
Magnesium: Nebulised MgSO4 has no role
Limited role for intravenous MgSO4
2 g Magnesium Sulphate in 100 mls of normal saline given intravenously over 20 minutes
Aminophylline: 5mg/kg over 20minutes loading dose
0.6mg/kg/hour IV infusion
If the patient is on maintenance take a baseline theophylline/ aminophylline level before maintenance infusion.
Furosemide: A theoretical bronchodilator of research interest, not better than nebulised ß2 agonists.
NIV:
There is limited evidence for NIV. This is not currently supported by the British Thoracic Society. The patient must be supervised by the intensivist that can proceed immediately to intubation.
There is limited evidence for NIV. This is not currently supported by the British Thoracic Society. The patient must be supervised by the intensivist that can proceed immediately to intubation.
Rapid Sequence Induction
Use at least a size 8.0 diameter
Ketamine --> 1-2mg/kg helps bronchodilate
Avoid atracurium
Disconnect circuit during CPR to allow chest to deflate
Bilateral thoracostomies.
Discharge
Non-pharmacological management:
Advise parents with asthma about the the dangers to their children of smoking.
Weight loss and breathing exercise programmes can help with asthma symptoms
Inhalers
Check technique
GP follow up within two working days of treatment
Steroids if PEFR initially <50% best or predicted.
Stop abruptly after five days as long as patient continues on inhaled steroids.
Careful discharging patients that present late in the evening or early hours of the morning since the airways are naturally at their narrowest at around 4am.
The British asthma guideline discourages routine antibiotic prescription in acute asthma. Infective triggers are most commonly viral.
Patients considered for discharge should meet all of the following criteria:
No life-threatening features at any point (including pre-hospital)
No features of severe asthma after initial treatment
PEFR >75% best or predicted and stable one hour after initial treatment
or
PEFR >50% best or predicted and stable two hours after initial treatment
Still have significant symptoms
Concern over compliance
Lives alone
Psychosocial problems
Physical disability or learning difficulties
History of severe asthma
Presentation at night
Pregnancy
Exacerbation despite adequate dose steroids pre-presentation
Two courses of systemic corticosteroids in the past year
Two or more attendances at the ED for their asthma in the past year
On step 4 or 5 of the BTS/SIGN guidelines treatment ladder
Who has childhood asthma with concurrent food allergy
Deaths
There's a national review of asthma deaths (NRAD). All deaths where asthma is on the death certificate at all need to be reported.
Tuesday, 4 November 2014
Asthma - Pathophysiology and Clinical Signs
Asthma is really common and affects lots of people. It also causes lots of unnecessary deaths, and a lot of hospital attendances from asthma attacks. The 2014 asthma guidelines replace the word "exacerbation" with "attack" as it's easier to understand.
References for this summary will be at the end of part two.
Physiology


Asthma is defined as a chronic airway inflammatory disorder with airway hyper-responsiveness.
Asthma is an obstructive lung condition, caused essentially by an allergic reaction to a trigger. Like most reactions, there is exposure that sensitizes the helper T cells, then IgE is produced, mast cells - and then you get the response on the second and subsequent exposure. The release of histamines and leukotrienes causes vasodilation, increased mucus secretion and bronchial smooth muscles contraction. The reaction also causes eosinophils to migrate into the airways, eyes and nose causing conjunctivitis, rhinitis and bronchiole constriction.
Clinical Features

The Calgary Guide has a nice summary here. There's no thing that says with 100% certainty that this is asthma.
These features increase the probability of asthma:
- >1 of wheeze, cough, difficulty breathing, chest tightness
- particularly if the symptoms:
are worse at night/early morning
occur in response to exercise, allergen exposure or cold air
are triggered by aspirin or beta-blockers
occur in the absence of a cold
- Personal or family history of atopic disorder or asthma
- Widespread wheeze on chest auscultation
- Otherwise unexplained low FEV1 or PEFR
- Otherwise unexplained peripheral blood eosinophilia
These features lower the probability of asthma:
- Symptoms with colds only
- Chronic productive cough without wheeze or breathlessness
- Dizzyness, light-headedness or paraesthesia peripherally
- Voice disturbance
- Cardiac disease
- Significant smoking history (>20 pack years)
- Repeated normal chest examination when symptomatic
- Repeatedly normal PEFR or spirometry when symptomatic
Grading Systems
The SIGN (and British Thoracic Society) guidelines use clinical symptoms to grade the severity of an attack in adults and children. The NICE guidelines appear to be based on the SIGN guidelines.
Systolic paradox (pulsus paradoxus), an historical marker of severity of asthma, is unhelpful and wastes valuable time so has been removed from the guidelines.
Features of patients at high risk of a life-threatening asthma attack:
Using a short-acting beta agonist inhaler more than once every four hours
Using more than one short-acting bronchodilator inhaler per month
Fewer than 12 prescriptions for preventer medication in the past year
Concurrent mental health problems
Investigations
Normally a clinical diagnosis, but if the patient has an intermediate probability of asthma, investigations can help. The Calgary guide has a summary.
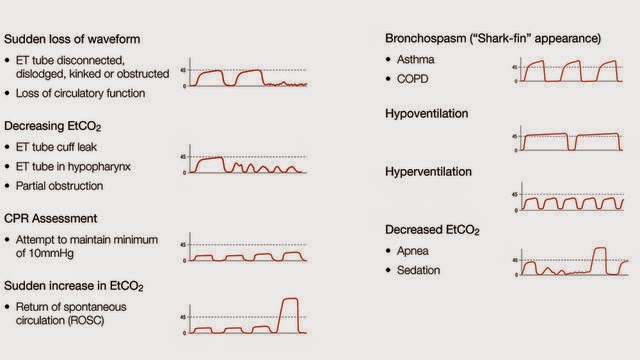
Capnography:
Wave form capnography should be used in acute exacerbations. Asthmatics get a "shark's fin" appearance because of the broncho-constriction.
Spirometry:
Spirometry shows reversibility and FEV1/FVC <0.7:
A decrease in FEV1 of > 15% after six minutes of exercise, or
An increase in FEV1 of > 15% after a two week trial of oral steroids (30 mg prednisolone once
daily), or
An increase in FEV1 of > 15% following therapy with a short acting beta 2 agonist
You can calculate the percentage change in FEV1 by:
Subtract the pre-bronchodilator FEV1 from the post-bronchodilator FEV1
Divide this by the pre-bronchodilator FEV1
Multiply by 100.
Peak Flow
60l/min. increase in PEFR) in response to either of the following strongly suggests underlying asthma:
400 mcg inhaled salbutamol
6-week trial of steroid inhaler (beclometasone 200 mcg bd or equivalent)
CXR
- Normal in up to 75% of patients
- pulmonary hyperinflation
- bronchial wall thickening - peribronchial cuffing
(non specific finding but may be present in ~48% of cases with asthma)
- pulmonary oedema due to asthma
CT
To look for complicated associated conditions such as allergic bronchopulmonary aspergillosis and not to directly diagnose asthma.
Non specific:
- bronchial wall thickening
- expiratory air trapping
- inspiratory decreased lung attenuation
- small centrilobular opacifities
- bronchial luminal narrowing - reduced
- bronchoarterial-diameter ratio
- sub segmental bronchiectasis - may be present in ~28-62% of asthmatics
Mimics
• Churg-Strauss
Look for signs and symptoms of systemic vasculitis, such as fever, weight loss, fatigue, and malaise, Be suspicious if there is a persistent eosinophilia, positive ANCA, and multiorgan involvement.
• COPD
• Anaphylaxis
4% of asthma admissions to PICU almost certainly had anaphylaxis rather than asthma - so make sure you consider it.
• Rhinitis
Management of chronic rhinosinusitis improves asthma control.
• Gastro-oesophageal reflux
Consider a three month trial of PPIs, as investigations to formally diagnose this are very invasive.
• Inhaled foreign body
• Airway stenosis
• Bronchiectasis
• Sarcoidosis
• Lung cancer
• Obliterative bronchioloitis
• Congestive cardiac
failure
• Pulmonary embolus
• Pulmonary fibrosis
• Hyperventilation syndrome
• Chronic cough syndrome
• Vocal cord dysfunction
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.
Saturday, 27 September 2014
Blood Gases
1. Anion Gap
(Na + K) - (Cl + HCO) Normal = 10 - 16mmol
>20 Primary metabolic acidosis regardless of pH or serum bicarbonate concentration
Low anion gap: dilution, low albumin, increased unmeasured cation (calcium, magnesium, lithium)
Non anion gap acidosis: HARD UPS
Hyperalimentation, acetazolamide, renal tubular acidosis, diarrhoea, uretero-pelvic shunt, post-hypocapnia, spironolactone
Raised Anion Gap: MUD PILES
Methanol, uraemia, DKA, paraldehyde, iron/ isoniazid, lactic acidosis, ethanol, ethylene glycol, salicylates
2. Excess Anion Gap = total anion gap - 12 + measured bicarb If >30 Metabolic alkalosis
If <23 Non gap metabolic acidosis
3. Delta Gap = Anion Gap - 12 (normal anion gap) < 0.4 Hyperchloraemic normal anion gap acidosis
< 1 High AG & normal AG acidosis
1 to 2 Pure Anion Gap Acidosis
Lactic acidosis: average value 1.6
DKA more likely to have a ratio closer to 1 due to urine ketone loss
> 2 High AG acidosis and a concurrent metabolic alkalosis or a pre-existing compensated respiratory acidosis
4. Osmolality - 2 (Na + K) + Glu + Urea
- Calculated vs measured should be 15- 20mmol / kg H20
- Elevation suggests the presence of exogenous osmotically active particles and includes 4 main groups:
Alcohols - Ethylene Glycol, methanol, ethanol, acetone, isopropyl alcohol
Sugars - Mannitol, Sorbitol
Lipids - e.g. hypertryglyceridaemia
Proteins - Hypergammaglobulinaemia
5. Expected CO2
The CO2 is a very swift compensatory change. The bicarb takes a while to change. This means you can use the bicarb to calculate what you would expect the CO2 to be. You can predict what you expect the CO2 to be. If it's not what you expect it to be, then there's a hidden acidosis or alkalosis.
Acute Respiratory Acidosis 1:10- The [HCO3] will increase by 1 mmol/l for every 10 mmHg elevation in pCO2 above 40 mmHg.
Expected [HCO3] = 24 + { (Actual pCO2 - 40) / 10 }
Chronic Respiratory Acidosis 4:10- The [HCO3] will increase by 4 mmol/l for every 10 mmHg elevation in pCO2 above 40mmHg.
Expected [HCO3] = 24 + 4 {(Actual pCO2 - 40) / 10}
Acute Respiratory Alkalosis 2:10
- The [HCO3] will decrease by 2 mmol/l for every 10 mmHg decrease in pCO2 below 40 mmHg.
Expected [HCO3] = 24 - 2 { ( 40 - Actual pCO2) / 10 }
Chronic Respiratory Alkalosis 5:10
Metabolic Acidosis 1 1/2 + 8
Expected pCO2 = 1.5 x [HCO3] + 8 (range: +/- 2)
Metabolic Alkalosis 0.7 + 20 Expected pCO2 = 0.7 [HCO3] + 20 (range: +/- 5)
6. Alveolar Gas Equation
Alveolar pO2 = inspired pO2 - arterial pCO2 x 1.2.
7. CausesRespiratory Alkalosis
Anxiety, pregnancy, hypoxia, sepsis, lung disease, hepatic encephalopathy, CNS disease, drugs
Respiratory Acidosis Acute airway obstruction, pulmonary embolism etc.
Metabolic AlkalosisVomiting, NG suction, diuretic use, post hyper-capnia
Excess mineralocorticoid activity, diuretics, excess alkali administration
Lactic Acidosis
- Ethylene glycol has a metabolite called glycolate, which is similar in structure to lactate. This can be wrongly interpreted by blood gas machines as an abnormally elevated lactate
- Sodium Bicarbonate is not routinely recommended. It can cause fluid overload, post recovery metabolic alkalosis, hypernatraemia. Often get rebound raise in CO2.
Venoarterial ParadoxDuring resuscitation and manual resuscitation, VBG and ABGs may be completely different. On the venous side of the circulation, the lungs are poorly perfused and there is a build up of CO2.
CO2 Units
from kPa to mmHg you multiply by 7.5
from mmHg to kPa you divide by 7.5
Pathophysiology Reminder
Chemoreceptors in the medulla and the carotid and aortic bodies sense changes in pCO2 and H+. This is then used to regulate alveolar ventilation. When ventilation rises, pCO2 falls. This occurs because ventilation lowers the alveolar pCO2 below that of mixed venous blood. CO2 molecules then diffuse into the alveolar gas, thus lowering the CO2 concentration in pulmonary capillary blood.
Shift to the right:
Alkalosis, raised pCO2, raised temperature, raised concentration of 2, 3-DPG
A shift to the left may be seen in:
Alkalosis, reduced pCO2, reduced temperature, reduced concentration of 2, 3-DPG
Henderson Hasselbach Equation : CO2 + H2O ? H2CO3 ? H+ + HCO3-
References
http://www.enlightenme.org/learning-zone/blood-gas-brain-freeze
http://www.enlightenme.org/the-curriculum-zone/diagnostics/blood-test-interpretation/arterial-blood-gas-analysis/learning-objectives
http://www.enlightenme.org/learning-zone/its-been-gas
http://www.enlightenme.org/learning-zone/alkalosis-has-gas-machine-broken-again
http://www.enlightenme.org/node/990/take
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1604
http://www.doctors.net.uk/ecme/wfrmNewIntro.aspx?moduleid=1512
http://lifeinthefastlane.com/ccc/arterial-blood-gas-in-hypothermia/
http://lifeinthefastlane.com/ccc/arterial-blood-gas-abg/
http://lifeinthefastlane.com/a-most-discombobulating-gas/http://learning.bmj.com/learning/modules/flow/JIT.html?execution=e1s1&locale=en_GB&action=start&sessionTimeoutInMin=90&moduleId=5004327&status=LIVE&_flowId=JIT
Friday, 26 September 2014
Pulmonary Embolism
PEs are the big diagnosis that we never want to miss, but we haven't yet decided the significance of all these tiny PEs we're picking up.
Statistics
PEs are very common: 60 to 70 per 100 000 population. They have an untreated mortality of about 30%, cause 15% of all postoperative deaths and are the most common cause of maternal death in the UK. 35 - 45% of thrombi are DVTs and up to 50% embolise. 65% of below knee DVTs are asymptomatic.
Pathogenesis:
Virchow's Triad:
Stasis: Immobility, surgery, casts
Vessel wall injury: trauma, sepsis, IVDA
Hyper-coaguable state: Primary Antithrombin and heparin cofactor II deficiencies
Protein C and S deficiencies
Factor V Leiden
Disorders of the fibrinolytic system
Lupus
Anticardiolipin antibodies
Prothrombin gene variant
Secondary Dehydration
Pregnancy
OCP
Malignancy
HONK
Risk Factors
* Major risk factors (relative risk increased 5-20-fold) include:
- Surgery - major and/or abdominal surgery
- Lower limb orthopaedic surgery, fracture or varicose veins.
- Obstetrics - late pregnancy (higher incidence with multiple births), caesarian section, pre-eclampsia
- Malignancy - pelvic, abdominal, metastatic (occult in 7 - 12% of patients)
- Previous proved VTE
- Reduced mobility - any major illness with prolonged bed rest.
* Minor risk factors (relative risk increased 2-4-fold) include:
- Cardiovascular - congenital heart disease, congestive cardiac failure, hypertension, central venous access
- Oestrogens - OCP (especially "third generation" pills), HRT (risk greatest in first year)
- Miscellaneous - occult malignancy, neurological disability, obesity, thrombotic and myeloproliferative disorders, nephrotic syndrome, inflammatory bowel disease.
* Inherited thrombophilias - need to interact with an additional risk factor to cause venous thromboembolism.
Clinical Signs & Symptoms
- Circulatory collapse in a previously well patient - happens in 5%.
Massive PE causes RHF.
Tachycardia in 30%.
- Pulmonary infarction syndrome (60%) -
pleuritic pain, with or without haemoptysis. Pleural rub.
- Isolated dyspnoea (25% - 73%) - sudden onset SOB
- Collapse, poor reserve (10%) -
In elderly patient with limited cardiorespiratory reserve. Small PE can be catastrophic.
- New onset AF and chest wall pain
- Prominent JVP “a” waves
- Right heart failure
- Pulmonary area murmur
May be completely normal, but tachycardia (classically with a loud P2 and splitting of the second heart sound) with tachypnoea are common
- Signs of a deep vein thrombosis are present in about 25%
Pregnancy
The diagnosis can be difficult to make in women who are pregnant. The standard pre-test clinical probability score should be used, recognising that pregnancy is a major risk factor for venous thromboembolism. The D-dimer test is of no use in this situation because it is raised (in the absence of PE) from about six weeks' gestation, until about three months post-partum.
The risk of pulmonary embolism increases throughout pregnancy, with more pulmonary emboli occurring after delivery than before. The risk of pulmonary embolism in pregnancy increases with maternal age and multiple births.
Pregnancy women normally have a mild compensated respiratory alkalosis.
Penicillins and cefalosporins safe in pregnancy. Avoid co-amox.
Pulmonary oedema higher risk in pregnant women because they have a lower serum osmotic pressure, and increased vascular permeability. Causes include pre-eclampsia, beta adrenergic agonists used to postpone premature labour, cardiac disease, amniotic fluid embolism.
Amniotic fluid embolism is typically associated with rapid changes in coagulation and evidence of DIC. PE does not cause such changes.
Investigations
* SI QIII TIII pattern - deep S wave in lead I, Q wave in III, inverted T wave in III.
20% of patients with PE.
* Chest x-ray: wedge shaped infarction or infection
regional oligaemia (Westermark sign)
pleural effusions
* ABG: Hypoxia results from reduced cardiac output and a low mixed PaO2 with ventilation/perfusion mismatching. A normal PaO2 and alveolar arterial gradient is possible in a young, healthy person.
Definitions
Massive PE: Acute PE with obstructive shock or SBP <90mmHg: at least 1 of the following:
- Sustained hypotension from PE itself (SBP < 90 mmHg for = 15 min, or requiring inotropic support)
- Pulselessness
- Persistent profound bradycardia (HR < 40 bpm with signs/symptoms of shock)
Submassive PE: Acute PE without systemic hypotension (SBP = 90 mmHg) but with either:
* RV dysfunction (of at least 1 of the following):
- RV dilation
- BNP > 90 pg/mL
- N-terminal pro-BNP > 500 pg/mL
- ECG changes: New complete or incomplete right BBB, anteroseptal ST elevation or depression, or anteroseptal T-wave inversion
• Myocardial necrosis is defined as either of the following:
- Troponin I > 0.4 ng/mL, or
- Troponin T > 0.1 ng/mL
Low Risk PE: Acute PE and the absence of the clinical markers of adverse prognosis
that define massive or sub-massive PE.
Scoring Systems
The original ‘PERC’ study excluded patients:
* patients in whom shortness of breath is not the most important, or equally most important, presenting complaint
* cancer
* thrombophilia or strong FHx
* beta blockers that may mask tachycardia
* transient tachycardia
* patients with amputations
* massively obese and in whom leg swelling cannot be reliably ascertained
* baseline hypoxemia
PERC rule can’t be used on: HAD CLOTS
Hormone, Age >50, DVT/PE history, Coughing blood, Leg swelling, O2 >95%, Tachycardia 100+, Surgery/trauma <28 d
Treatment
Massive PE - Alteplase 50mg ASAP.
Anticoagulation for three or six months for a first idiopathic pulmonary embolism. A British Thoracic Society trial comparing three and six months' treatment is ongoing. Some trusts use PESI to work out whether outpatient anticoagulation is suitable.

Flight prophylaxis. Current British guidelines suggest considering aspirin or LMWH, or formal anticoagulation for those at high risk of pulmonary embolism. Limited evidence to support this. Compression stockings may be beneficial.
Differentials
Venous air emboli may cause:
Raised venous pressure
Cyanosis
Hypotension
Tachycardia
Syncope.
Treatment is by lying the patient on their right side, with head down and feet up, to allow air to collect and stay at the cardiac apex. From here it can be aspirated. This may be done by ultrasound guided needle aspiration.
Fat embolism
This occurs in association with long bone fractures, with bone marrow fat droplets released into the venous circulation at fracture. It is more common in non-immobilised fractures.
It typically presents with:
Hypoxia
Coagulopathy
Transient petechial rash on neck, axillae, and skin folds
Neurological disturbance, such as confusion.
Fat globules can be identified in the urine.
Treatment is supportive.
References
http://www.enlightenme.org/knowledge-bank/cempaedia/pulmonary-embolism
http://lifeinthefastlane.com/education/ccc/pulmonary-embolism/
http://lifeinthefastlane.com/ecg-library/pe/
http://lifeinthefastlane.com/cicm-saq-2012-2-q5/http://lifeinthefastlane.com/education/ccc/thrombolysis-submassive-pulmonary-embolus/
http://lifeinthefastlane.com/cardiovascular-curveball-011/
http://lifeinthefastlane.com/pulmonary-puzzle-016/
http://lifeinthefastlane.com/hematology-hoodwinker-001/
http://www.enlightenme.org/the-curriculum-zone/node/2091http://www.enlightenme.org/the-curriculum-zone/node/11779http://m.eurheartj.oxfordjournals.org/content/early/2014/09/17/eurheartj.ehu283
Statistics
PEs are very common: 60 to 70 per 100 000 population. They have an untreated mortality of about 30%, cause 15% of all postoperative deaths and are the most common cause of maternal death in the UK. 35 - 45% of thrombi are DVTs and up to 50% embolise. 65% of below knee DVTs are asymptomatic.
Pathogenesis:
Virchow's Triad:
Stasis: Immobility, surgery, casts
Vessel wall injury: trauma, sepsis, IVDA
Hyper-coaguable state: Primary Antithrombin and heparin cofactor II deficiencies
Protein C and S deficiencies
Factor V Leiden
Disorders of the fibrinolytic system
Lupus
Anticardiolipin antibodies
Prothrombin gene variant
Secondary Dehydration
Pregnancy
OCP
Malignancy
HONK
Risk Factors
* Major risk factors (relative risk increased 5-20-fold) include:
- Surgery - major and/or abdominal surgery
- Lower limb orthopaedic surgery, fracture or varicose veins.
- Obstetrics - late pregnancy (higher incidence with multiple births), caesarian section, pre-eclampsia
- Malignancy - pelvic, abdominal, metastatic (occult in 7 - 12% of patients)
- Previous proved VTE
- Reduced mobility - any major illness with prolonged bed rest.
* Minor risk factors (relative risk increased 2-4-fold) include:
- Cardiovascular - congenital heart disease, congestive cardiac failure, hypertension, central venous access
- Oestrogens - OCP (especially "third generation" pills), HRT (risk greatest in first year)
- Miscellaneous - occult malignancy, neurological disability, obesity, thrombotic and myeloproliferative disorders, nephrotic syndrome, inflammatory bowel disease.
* Inherited thrombophilias - need to interact with an additional risk factor to cause venous thromboembolism.
Clinical Signs & Symptoms
Massive PE causes RHF.
Tachycardia in 30%.
- Pulmonary infarction syndrome (60%) -
pleuritic pain, with or without haemoptysis. Pleural rub.
- Isolated dyspnoea (25% - 73%) - sudden onset SOB
- Collapse, poor reserve (10%) -
In elderly patient with limited cardiorespiratory reserve. Small PE can be catastrophic.
- New onset AF and chest wall pain
- Prominent JVP “a” waves
- Right heart failure
- Pulmonary area murmur
May be completely normal, but tachycardia (classically with a loud P2 and splitting of the second heart sound) with tachypnoea are common
- Signs of a deep vein thrombosis are present in about 25%
Pregnancy
The diagnosis can be difficult to make in women who are pregnant. The standard pre-test clinical probability score should be used, recognising that pregnancy is a major risk factor for venous thromboembolism. The D-dimer test is of no use in this situation because it is raised (in the absence of PE) from about six weeks' gestation, until about three months post-partum.
The risk of pulmonary embolism increases throughout pregnancy, with more pulmonary emboli occurring after delivery than before. The risk of pulmonary embolism in pregnancy increases with maternal age and multiple births.
Pregnancy women normally have a mild compensated respiratory alkalosis.
Penicillins and cefalosporins safe in pregnancy. Avoid co-amox.
Pulmonary oedema higher risk in pregnant women because they have a lower serum osmotic pressure, and increased vascular permeability. Causes include pre-eclampsia, beta adrenergic agonists used to postpone premature labour, cardiac disease, amniotic fluid embolism.
Amniotic fluid embolism is typically associated with rapid changes in coagulation and evidence of DIC. PE does not cause such changes.
Investigations
* SI QIII TIII pattern - deep S wave in lead I, Q wave in III, inverted T wave in III.
20% of patients with PE.
* Chest x-ray: wedge shaped infarction or infection
regional oligaemia (Westermark sign)
pleural effusions
* ABG: Hypoxia results from reduced cardiac output and a low mixed PaO2 with ventilation/perfusion mismatching. A normal PaO2 and alveolar arterial gradient is possible in a young, healthy person.
Definitions
Massive PE: Acute PE with obstructive shock or SBP <90mmHg: at least 1 of the following:
- Sustained hypotension from PE itself (SBP < 90 mmHg for = 15 min, or requiring inotropic support)
- Pulselessness
- Persistent profound bradycardia (HR < 40 bpm with signs/symptoms of shock)
Submassive PE: Acute PE without systemic hypotension (SBP = 90 mmHg) but with either:
* RV dysfunction (of at least 1 of the following):
- RV dilation
- BNP > 90 pg/mL
- N-terminal pro-BNP > 500 pg/mL
- ECG changes: New complete or incomplete right BBB, anteroseptal ST elevation or depression, or anteroseptal T-wave inversion
• Myocardial necrosis is defined as either of the following:
- Troponin I > 0.4 ng/mL, or
- Troponin T > 0.1 ng/mL
Low Risk PE: Acute PE and the absence of the clinical markers of adverse prognosis
that define massive or sub-massive PE.
Scoring Systems
The original ‘PERC’ study excluded patients:
* patients in whom shortness of breath is not the most important, or equally most important, presenting complaint
* cancer
* thrombophilia or strong FHx
* beta blockers that may mask tachycardia
* transient tachycardia
* patients with amputations
* massively obese and in whom leg swelling cannot be reliably ascertained
* baseline hypoxemia
PERC rule can’t be used on: HAD CLOTS
Hormone, Age >50, DVT/PE history, Coughing blood, Leg swelling, O2 >95%, Tachycardia 100+, Surgery/trauma <28 d
Treatment
Massive PE - Alteplase 50mg ASAP.
Anticoagulation for three or six months for a first idiopathic pulmonary embolism. A British Thoracic Society trial comparing three and six months' treatment is ongoing. Some trusts use PESI to work out whether outpatient anticoagulation is suitable.

Flight prophylaxis. Current British guidelines suggest considering aspirin or LMWH, or formal anticoagulation for those at high risk of pulmonary embolism. Limited evidence to support this. Compression stockings may be beneficial.
Differentials
Venous air emboli may cause:
Raised venous pressure
Cyanosis
Hypotension
Tachycardia
Syncope.
Treatment is by lying the patient on their right side, with head down and feet up, to allow air to collect and stay at the cardiac apex. From here it can be aspirated. This may be done by ultrasound guided needle aspiration.
Fat embolism
This occurs in association with long bone fractures, with bone marrow fat droplets released into the venous circulation at fracture. It is more common in non-immobilised fractures.
It typically presents with:
Hypoxia
Coagulopathy
Transient petechial rash on neck, axillae, and skin folds
Neurological disturbance, such as confusion.
Fat globules can be identified in the urine.
Treatment is supportive.
References
http://www.enlightenme.org/knowledge-bank/cempaedia/pulmonary-embolism
http://lifeinthefastlane.com/education/ccc/pulmonary-embolism/
http://lifeinthefastlane.com/ecg-library/pe/
http://lifeinthefastlane.com/cicm-saq-2012-2-q5/http://lifeinthefastlane.com/education/ccc/thrombolysis-submassive-pulmonary-embolus/
http://lifeinthefastlane.com/cardiovascular-curveball-011/
http://lifeinthefastlane.com/pulmonary-puzzle-016/
http://lifeinthefastlane.com/hematology-hoodwinker-001/
http://www.enlightenme.org/the-curriculum-zone/node/2091http://www.enlightenme.org/the-curriculum-zone/node/11779http://m.eurheartj.oxfordjournals.org/content/early/2014/09/17/eurheartj.ehu283
Tuesday, 23 September 2014
HAP6
Respiratory and Breathing problems basically covers:
Asthma
Pulmonary embolism - including echo
COPD and NIV
Aspiration
Pneumonia
Pulmonary Oedema
Pneumothorax
Dysproportionate hyperventilation
Pleural effusion
Inhalation
ABG interpretation
CXR interpretation
Asthma
Pulmonary embolism - including echo
COPD and NIV
Aspiration
Pneumonia
Pulmonary Oedema
Pneumothorax
Dysproportionate hyperventilation
Pleural effusion
Inhalation
ABG interpretation
CXR interpretation
Tuesday, 10 June 2014
Dialysis
Dialysis is surprisingly difficult to find information
about. In the emergency department, I think we're only
interested in:
- how do we not look stupid when a renal patient comes in
- which patients do we need to arrange urgent dialysis for
- what do we do differently with a sick patient on dialysis
Overview
There are two main types of "routine" dialysis. In ICU it is different, and their dialysis is normally continuous, and there are many different types.
- Haemodialysis
Fine fibre tubes mimic the body's glomeruli, and filter the blood. Semi permiable. Waste products carried away. You need hydrostatic pressure to be able to increase.
- Peritoneal dialysis
Dialysis fluid introduced into the adbdominal cavity. Waste transfers through the peritoneal membrane into the fluid. Abdomen then drained. Could be continuous ambulatory peritoneal dialysis - which doesn't need a machine, or continuous cycler-assisted peritoneal dialysis.
Urgent Dialysis
I think the most common cause of urgent dialysis from the ED is hyperkalaemia, and potentially drug overdose. Dialysis might also be indicated for pulmonary oedema.
Not all drugs are dialysed out successfully.
Sick Dialysis Patient
- Speak to their renal unit
- Check electrolytes
- Fluid overload normally needs dialysis, as diuretics need functioning kidneys
- Infection is a leading cause of death - always send cultures. Pyrexia is often related to gram positive sepsis.
- Anticoagulation - renal failure often leads to a bleeding tendency. Ask which anticoagulants have been used.
- Dialysis related hypotension is the most frequent symptomatic complication. It is caused by reflex withdrawal of sympathetic tone resulting from reduced left ventricular filling. This normally happens because the patient's fluid balance is suboptimal.
- Cramps are common and might be due to volume depletion and tissue hypoxia. Hypertonic fluid, like 50mls of 50% dextrose often raises plasma osmolality and helps.
- The most serious acute events during dialysis include air embolism, line disconnection leading to haemorrhage, acute haemolysis or toxicity related to line kinking or dialysis contamination, and acute allergic reactions to dialysers or sterilants (ethylene oxide).
Lines
Don't touch the fistula. When cannulating use veins as distal as possible, to try and preserve the bigger access.
Bleeding fistula are often caused by infection. They need compression, possibly topical tranexamic acid, and urgent vascular referral.
References
http://ccforum.com/content/pdf/cc10280.pdf
http://lifeinthefastlane.com/tag/dialysis/
https://www.emrap.org/episode/2013/april/thehypotensive
http://www.emlitofnote.com/2011/12/risks-of-missing-dialysis.html
http://academiclifeinem.com/mythbuster-urgent-dialysis-following-iv-contrast/
http://www.kidneydialysis.org.uk/hemodialysis.htm
http://www.kidneyatlas.org/book5/adk5-01.ccc.QXD.pdf
http://www.edrep.org/pages/textbook/haemodialysis.php
http://openmed.co.uk/curriculum/renal/
http://www.frca.co.uk/article.aspx?articleid=100367
http://www.frca.co.uk/Documents/194%20Renal%20replacement%20therapy%20in%20critical%20care.pdf
http://www.learnicu.org/Presentations/RRT%20in%20ICU.ppt
http://www.ccmtutorials.com/renal/rrt/index.htm
- how do we not look stupid when a renal patient comes in
- which patients do we need to arrange urgent dialysis for
- what do we do differently with a sick patient on dialysis
Overview
There are two main types of "routine" dialysis. In ICU it is different, and their dialysis is normally continuous, and there are many different types.
- Haemodialysis
Fine fibre tubes mimic the body's glomeruli, and filter the blood. Semi permiable. Waste products carried away. You need hydrostatic pressure to be able to increase.
- Peritoneal dialysis
Dialysis fluid introduced into the adbdominal cavity. Waste transfers through the peritoneal membrane into the fluid. Abdomen then drained. Could be continuous ambulatory peritoneal dialysis - which doesn't need a machine, or continuous cycler-assisted peritoneal dialysis.
Urgent Dialysis
I think the most common cause of urgent dialysis from the ED is hyperkalaemia, and potentially drug overdose. Dialysis might also be indicated for pulmonary oedema.
Not all drugs are dialysed out successfully.
Sick Dialysis Patient
- Speak to their renal unit
- Check electrolytes
- Fluid overload normally needs dialysis, as diuretics need functioning kidneys
- Infection is a leading cause of death - always send cultures. Pyrexia is often related to gram positive sepsis.
- Anticoagulation - renal failure often leads to a bleeding tendency. Ask which anticoagulants have been used.
- Dialysis related hypotension is the most frequent symptomatic complication. It is caused by reflex withdrawal of sympathetic tone resulting from reduced left ventricular filling. This normally happens because the patient's fluid balance is suboptimal.
- Cramps are common and might be due to volume depletion and tissue hypoxia. Hypertonic fluid, like 50mls of 50% dextrose often raises plasma osmolality and helps.
- The most serious acute events during dialysis include air embolism, line disconnection leading to haemorrhage, acute haemolysis or toxicity related to line kinking or dialysis contamination, and acute allergic reactions to dialysers or sterilants (ethylene oxide).
Lines
Don't touch the fistula. When cannulating use veins as distal as possible, to try and preserve the bigger access.
Bleeding fistula are often caused by infection. They need compression, possibly topical tranexamic acid, and urgent vascular referral.
References
http://ccforum.com/content/pdf/cc10280.pdf
http://lifeinthefastlane.com/tag/dialysis/
https://www.emrap.org/episode/2013/april/thehypotensive
http://www.emlitofnote.com/2011/12/risks-of-missing-dialysis.html
http://academiclifeinem.com/mythbuster-urgent-dialysis-following-iv-contrast/
http://www.kidneydialysis.org.uk/hemodialysis.htm
http://www.kidneyatlas.org/book5/adk5-01.ccc.QXD.pdf
http://www.edrep.org/pages/textbook/haemodialysis.php
http://openmed.co.uk/curriculum/renal/
http://www.frca.co.uk/article.aspx?articleid=100367
http://www.frca.co.uk/Documents/194%20Renal%20replacement%20therapy%20in%20critical%20care.pdf
http://www.learnicu.org/Presentations/RRT%20in%20ICU.ppt
http://www.ccmtutorials.com/renal/rrt/index.htm
Subscribe to:
Comments (Atom)