We use lactate a lot, and it is mentioned specifically in the syllabus - it says we should be able to "understand the significance of lactic acidosis in the critically ill patient".
Pathophysiology
Lactate is produced by glycolysis and metabolised by the liver. It is commonly thought it is produced as a result of anaerobic metabolism, but this has been disproved. It is now thought that the adrenergic state and cytokine storm probably change glucose metabolism, changing lactate production.
Adrenaline stimulates beta-2 receptors which up-regulates glycolysis, generating more pyruvate than can be used by the cell’s mitochondria. This excess pyruvate is converted into lactate.
Lactate can be used by the heart and brain as a fuel source, further suggesting lactate is a stress response.
Lactate clearance is reduced in hepatic failure. The utility of lactate clearance as a marker of disease severity is debated. Some suggest if the lactate level doesn't drop, lactate must still be being produced - so things are serious. The half life of lactate is about twenty minutes.
Measuring Lactate
The lactate level is independent of anion gap and bicarb so does need to be checked. The level can be high, even if the blood pressure is low.
A venous level is fine, unless there's been a really prolonged tourniquet time when taking the sample!
If you're sending your tests to the lab, even at room temperature (not on ice) the value doesn't change).
Causes of High (>4) lactate
Sepsis
Exercise
Beta-agonist use (like salbutamol)
Even not on ice, the lactate value is unchanged for 15minutes at room temperature.
Treating a High Lactate
Identify and treat the cause - it's not always sepsis
Remember, a high lactate is a marker of disease severity, not a marker of disease.
Hartmann's (ringers lactate) does not contain the right type of lactate, and does not affect the lactate level.
Remember nebulisers can cause a high latate - which might worsen the dyspnoea.
Causes of a High Lactate
Type A lactic acidosis is seen in states of hypoperfusion or poor oxygenation - shock and cardiac arrest
Type B lactic acidosis is seen in states of high metabolism, organ dysfunction, and toxins. This might be contributed to by thiamine deficiency, neoplastic cells, mitochondrial dysfunction (antiretroviral therapy, linezolid, propofol), hepatic dysfunction.
I haven't written a summary on this one - I think St Emlyns have summarised quite well!!
References
http://emcrit.org/pulmcrit/understanding-lactate-in-sepsis-using-it-to-our-advantage/
http://www.emdocs.net/utility-obtaining-lactate-measurement-ed/
http://emj.bmj.com/content/32/9/670.full?hwoasp=authn%3A1451324344%3A4223703%3A1415336879%3A0%3A0%3AVUcQvREASLSBBNQdFnX7Aw%3D%3D
http://emcrit.org/wee/lactate-clearance-flawed/
http://www.heftemcast.co.uk/lactate-lactate-clearance/
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4427204/
http://emnerd.com/tag/lactate-clearance/
http://emcrit.org/wp-content/uploads/lactate-faq.pdf
http://www.rcemfoamed.co.uk/portfolio/sepsis-in-the-ed/
http://www.aliem.com/blast-from-the-past-occult-sepsis-lactic-acid-and-mortality/
http://www.oapublishinglondon.com/article/431#
http://emcrit.org/wee/lactate-clearance-flawed/
http://www.ncbi.nlm.nih.gov/pubmed/9366769
Sunday 27 December 2015
Tuesday 28 July 2015
Right Sided Heart Failure
It's often difficult to differentiate right sided heart failure from left sided - because left goes on to cause right!
Pathophysiology
P Waves:
Pathophysiology
Caused by respiratory problems, and by progression of left sided heart failure.
Signs
High JVP
Pitting oedema
RUQ pain - hepatomegaly
Loud P2, and heave
Investigations
ECG: If the ECG is normal, heart failure is unlikely
Reduced ECG amplitude (more air between heart and leads)
Prominent P waves
Right axis deviation
RBBB (Broad QRS > 120 ms, RSR’ pattern in V1-3 (‘M-shaped’ QRS complex), Wide, slurred S wave in the lateral leads (I, aVL, V5-6))
Sagging of ST segment below baseline
| http://lifeinthefastlane.com/ecg-library/basics/p-wave/ |
P Waves:
P mitrale (bifid P waves), seen with left atrial enlargement.
P pulmonale (peaked P waves), seen with right atrial enlargement.
P wave inversion, seen with ectopic atrial and junctional rhythms.
Variable P wave morphology, seen in multifocal atrial rhythms.
--> if P waves are inverted check lead placement
Management
Reduce hypoxia and hypercarbia
Ventilation and PEEP
Inotropes and vasopressors
RV assist device may be useful
http://lifeinthefastlane.com/ecg-library/copd/
http://lifeinthefastlane.com/ecg-library/basics/p-wave/
http://lifeinthefastlane.com/ccc/right-ventricular-failure/
http://www.rcemlearning.co.uk/references/pulmonary-hypertension-and-right-heart-failure/
http://www.rcemlearning.co.uk/references/pulmonary-hypertension-and-right-heart-failure/
http://www.rcemfoamed.co.uk/portfolio/rcem-belfast-day-3/
Left Heart Failure
Pathophysiology
The left side of the heart fails, for many reasons:
- Restrictive (haemochromatosis, pericardial disease)
- Ischaemic (MI)
- Congestive (volume overload of teventricle from valvular insufficiencies)
- Hypertrophic (longstanding HTN)
SV affected by preload, afterload and myocardial contractility. The Frank-Starling Curve has an effect here.
Symptoms
Exertional dyspnoea
Fatigue
PND
Orthopnoea
Vague "not feeling right"
Clinical Findings
- Increased sympathetic activity to attempt to maintain cardiac output = sweating, tachypnoea, tachycardia
- Loud P2, presence of S3 and S4
- Raised diastolic pressure --> narrowed pulse pressure
- Ascites
- Ankle oedema
Investigations
BNP
<100 microgram /mL - unlikely CHF
100 - 500 = may be CHF
500 - most consistent with CHF
CXR
Upper lobe diversion
Peri-bronchial cuffing
Kerley B lines
White interlobular fissures
Pleural effusion
Air bronchogram
Airspace opacification
Cardiomegaly - cardiac ratio > 0.5 on PA film
Echo
Look for evidence of ischaemia and poor contractility
Management Options
Decrease Pre-load: Salt and water restriction
Reduce caffeine, alcohol and smoking
Diuretics - get euvolemia, then titrate to lowest possible dose.
Improve contractility: Inotropes
Reduce afterload: Vasodilators
Improve Mortality:
- ACE inhibitors eg. ramipril - NNT 26. Titrate up
- Angiotensin receptor blockers if ACE intolerant.
- Beta blockers eg. metoprolol
- Consider aldosterone agonists like spironolactone NNT 10 or eplerenone NNT 34
End of Life
There is no cure - consider end of life options early. Involve palliative care if needed.
Grading
Class I
No limitations, ordinary physical activity does not cause undue fatigue, dyspnoea or palpitations (asymptomatic LV dysfunction). 5% 1 year mortality.
Class II
Slight limitation of physical activity, ordinary physical activity results in fatigue, palpitation, dyspnoea, or angina (Mild CHF). 10% 1 year mortality.
Class III
Marked limitation of physical activity. Less than ordinary physical activity causes symptoms (moderate CHF). 20% 1 year mortality.
Class IV
Unable to carry on any physical activity without discomfort. Symptoms of CHF present at rest (severe CHF). 50% 1 year mortality.
References
http://www.cemfoamed.co.uk/portfolio/agm-conference/
http://learning.bmj.com/learning/module-intro/chronic-heart-failure.html?moduleId=10051928&searchTerm=%E2%80%9Cheart%20failure%E2%80%9D&page=1&locale=en_GB
http://lifeinthefastlane.com/frank-starling-curve-physiology-bscc/
http://calgaryguide.ucalgary.ca/left-heart-failure-pathogenesis/
http://foam4gp.com/2014/10/23/chronic-heart-failure/
The left side of the heart fails, for many reasons:
- Restrictive (haemochromatosis, pericardial disease)
- Ischaemic (MI)
- Congestive (volume overload of teventricle from valvular insufficiencies)
- Hypertrophic (longstanding HTN)
This reduces the stroke volume, and hence the cardiac output.
Cardiac output = stroke volume x heart rateSV affected by preload, afterload and myocardial contractility. The Frank-Starling Curve has an effect here.
Exertional dyspnoea
Fatigue
PND
Orthopnoea
Vague "not feeling right"
Clinical Findings
- Increased sympathetic activity to attempt to maintain cardiac output = sweating, tachypnoea, tachycardia
- Loud P2, presence of S3 and S4
- Raised diastolic pressure --> narrowed pulse pressure
- Ascites
- Ankle oedema
Investigations
BNP
<100 microgram /mL - unlikely CHF
100 - 500 = may be CHF
500 - most consistent with CHF
CXR
Upper lobe diversion
Peri-bronchial cuffing
Kerley B lines
White interlobular fissures
Pleural effusion
Air bronchogram
Airspace opacification
Cardiomegaly - cardiac ratio > 0.5 on PA film
Echo
Look for evidence of ischaemia and poor contractility
Management Options
Decrease Pre-load: Salt and water restriction
Reduce caffeine, alcohol and smoking
Diuretics - get euvolemia, then titrate to lowest possible dose.
Improve contractility: Inotropes
Reduce afterload: Vasodilators
Improve Mortality:
- ACE inhibitors eg. ramipril - NNT 26. Titrate up
- Angiotensin receptor blockers if ACE intolerant.
- Beta blockers eg. metoprolol
- Consider aldosterone agonists like spironolactone NNT 10 or eplerenone NNT 34
End of Life
There is no cure - consider end of life options early. Involve palliative care if needed.
Grading
Class I
No limitations, ordinary physical activity does not cause undue fatigue, dyspnoea or palpitations (asymptomatic LV dysfunction). 5% 1 year mortality.
Class II
Slight limitation of physical activity, ordinary physical activity results in fatigue, palpitation, dyspnoea, or angina (Mild CHF). 10% 1 year mortality.
Class III
Marked limitation of physical activity. Less than ordinary physical activity causes symptoms (moderate CHF). 20% 1 year mortality.
Class IV
Unable to carry on any physical activity without discomfort. Symptoms of CHF present at rest (severe CHF). 50% 1 year mortality.
References
http://www.cemfoamed.co.uk/portfolio/agm-conference/
http://learning.bmj.com/learning/module-intro/chronic-heart-failure.html?moduleId=10051928&searchTerm=%E2%80%9Cheart%20failure%E2%80%9D&page=1&locale=en_GB
http://lifeinthefastlane.com/frank-starling-curve-physiology-bscc/
http://calgaryguide.ucalgary.ca/left-heart-failure-pathogenesis/
http://foam4gp.com/2014/10/23/chronic-heart-failure/
Friday 26 June 2015
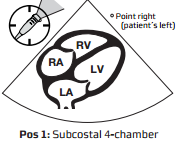
Echo in Life Support
One of the competencies we have to get is echo in life support. I've floated around with echo for a while - but now it's time to knuckle down and be 100% excellent at what we need to do to be level one competent.
- Subxiphoid + one other view, normally parasternal long axis
- Identifies pericardial space
- Look at LV RV (?dilated)
- Identifies IVC, looks at diameter and assesses collapsibility
The Probe
If you are using a cardiac probe, the marker (dot) needs to be on the right to give you the views you are used to. This means that mostly, the probe is near the apex of the heart If you are using an abdominal probe (as many of us have to, especially for the subcostal view) the dot will be on the left.
The Anatomy
Remember that the heart doesn't lie exactly vertically. It lies tilted, and slanted. This helps you to think about what you are seeing.
Subxiphoid or Subcostal View
This is similar to an apical view, but everything is rotated 90 degrees. You can use a curved probe to get this view. Imagine you are shining a torch on the heart. Point it down, and to the patient's left. Remember, the right hand side of the heart is next to the liver.
Because the heart is tilted slightly, the probe hits the liver first, then the right hand side of the heart, and then the left hand side - hence the view you get with the right side of the heart at the top, and the left at the bottom.
Fluid normally collects posteriorly. This view is really good for looking at fluid.
Parasternal Long axis
Aim the probe perpendicular to the chest, just to the left of the sternum in the 4-5th IC space (although I was told that the third is better). The marker should be pointing to the top of the patient. Point towards the patient's right shoulder.
This is really good for looking at LV function, and also shows effusions well.
Remember that the right atrium is likely to be hiding behind the aortic outlet.
Parasternal Short Axis
Rotate the probe to look at the patient's left shoulder, keeping the probe marker on the patient's left. This gives you a view at the bottom of the heart - looking at the ventricles.
If you scan at the level of the mitral valve, you get the croissant and doughnut appearance. You also get the fish mouth. This is the view we are aiming to get.
Apical Four and Five Chamber Views
Both of these views have the probe in the same sort of position. To get a five chamber view, you point the probe down a little more to be able to see the aorta. The probe marker is on the patient's left.
IVC
Remember that this will be affected by your probe. Start with a subxiphoid view. Rotate the probe vertically, with the probe marker (using a cardiac probe) at the top. Slide 1-2 cm to the right, and tilt towards the heart. This will give you a view of the liver, with the IVC below it, entering the right atrium.
Measure the heart where the hepatic vein is, or 2-3 cm from the heart edge.
Turn into M mode.
The IVC should collapse on inspiration. If it doesn't, ask the patient to sniff. Measure this as a percentage. If it collapses 25- 50%, they will be fluid tolerant. >50% very likely to be fluid responsive, some say >30%.
I was really struggling to get my head around this anatomy, and one of my collegues drew this brilliant picture for me - and it's mostly clicked. The key I think is thinking about how the heart lies (ie not straight!) and how your probe is looking.
References
http://emergencyultrasound.org.uk/resources/03+Cardiac+views+web.pdf
http://www.rcem.ac.uk/Training-Exams/Training/Ultrasound%20training
http://www.rcem.ac.uk/code/document.asp?ID=5447
https://www.youtube.com/watch?v=oMwgUo6sbyY
https://web.stanford.edu/group/ccm_echocardio/cgi-1bin/mediawiki/index.php/Subcostal_4_chamber_view
http://www.fate-protocol.com/130067GE_Fate_Card.pdf
http://www.smacc.net.au/sonowars-chicago/
http://lifeinthefastlane.com/own-the-echo/
- Subxiphoid + one other view, normally parasternal long axis
- Identifies pericardial space
- Look at LV RV (?dilated)
- Identifies IVC, looks at diameter and assesses collapsibility
The Probe
If you are using a cardiac probe, the marker (dot) needs to be on the right to give you the views you are used to. This means that mostly, the probe is near the apex of the heart If you are using an abdominal probe (as many of us have to, especially for the subcostal view) the dot will be on the left.
The Anatomy
Remember that the heart doesn't lie exactly vertically. It lies tilted, and slanted. This helps you to think about what you are seeing.
Subxiphoid or Subcostal View
Because the heart is tilted slightly, the probe hits the liver first, then the right hand side of the heart, and then the left hand side - hence the view you get with the right side of the heart at the top, and the left at the bottom.
Fluid normally collects posteriorly. This view is really good for looking at fluid.
Parasternal Long axis
Aim the probe perpendicular to the chest, just to the left of the sternum in the 4-5th IC space (although I was told that the third is better). The marker should be pointing to the top of the patient. Point towards the patient's right shoulder.
This is really good for looking at LV function, and also shows effusions well.
Remember that the right atrium is likely to be hiding behind the aortic outlet.
Parasternal Short Axis
Rotate the probe to look at the patient's left shoulder, keeping the probe marker on the patient's left. This gives you a view at the bottom of the heart - looking at the ventricles.
If you scan at the level of the mitral valve, you get the croissant and doughnut appearance. You also get the fish mouth. This is the view we are aiming to get.
Apical Four and Five Chamber Views
Both of these views have the probe in the same sort of position. To get a five chamber view, you point the probe down a little more to be able to see the aorta. The probe marker is on the patient's left.
IVC
Remember that this will be affected by your probe. Start with a subxiphoid view. Rotate the probe vertically, with the probe marker (using a cardiac probe) at the top. Slide 1-2 cm to the right, and tilt towards the heart. This will give you a view of the liver, with the IVC below it, entering the right atrium.
Measure the heart where the hepatic vein is, or 2-3 cm from the heart edge.
Turn into M mode.
The IVC should collapse on inspiration. If it doesn't, ask the patient to sniff. Measure this as a percentage. If it collapses 25- 50%, they will be fluid tolerant. >50% very likely to be fluid responsive, some say >30%.
I was really struggling to get my head around this anatomy, and one of my collegues drew this brilliant picture for me - and it's mostly clicked. The key I think is thinking about how the heart lies (ie not straight!) and how your probe is looking.
References
http://emergencyultrasound.org.uk/resources/03+Cardiac+views+web.pdf
http://www.rcem.ac.uk/Training-Exams/Training/Ultrasound%20training
http://www.rcem.ac.uk/code/document.asp?ID=5447
https://www.youtube.com/watch?v=oMwgUo6sbyY
https://web.stanford.edu/group/ccm_echocardio/cgi-1bin/mediawiki/index.php/Subcostal_4_chamber_view
http://www.fate-protocol.com/130067GE_Fate_Card.pdf
http://www.smacc.net.au/sonowars-chicago/
http://lifeinthefastlane.com/own-the-echo/
Monday 8 June 2015
Sore Throat - Tonsillitis
Most sore throats are not caused by a bacterial infection. Make sure there is no epiglottitis or scarlet fever. Scarlet fever would be seen with a rough textured macular rash, with Pastia's lines, and red cheeks with perioral sparing.
There could also be Lemierre's syndrome, retropharyngeal abscess, diptheria, bacterial tracheitis, Ludwig's angina or angioedema.
Red flags for sore throat including significant systemic upset, severe pain, stridor, severe neck stiffness, inability to swallow or tripod position.
Causes
Group A β haemolytic streptococcus - 5-15%
Can cause rheumatic fever in some patients, toxic shock syndrome, necrotising fascitis and post-strep glomerulonephritis. GABHS can be carried asymptomatically - mostly between 3 and 15yrs old (carriage rates 5 - 21%). Adults have much lower carriage rates.
Complications can be suppurative (otitis media, sinusitis, peritonsillar abscess) or non-suppurative (rheumatic fever).
Treat with pen V, 500mg QDS for 10 days.
Viral Tonsillitis
Tonsillitis/pharyngitis are: rhinovirus; coronavirus; adenovirus; herpes simplex; parainfluenza; echovirus; coxsackie A; Epstein-Barr; CMV.
Epstein-Barr Virus
This causes infectious mononucleosis which presents with malaise, headache, fever, pharyngitis, posterior cervical node enlargement, splenomegaly and hepatomegaly. There is a lethargy lasting for six to eight weeks, with suffers being infective for weeks to months. Glandular fever causes anterior and posterior chain lymphadenopathy - bacterial is normally just the upper anterior cervical chain.
Diagnosis is supported by monospot, and there may be atypical lymphocytes and deranged liver enzymes.
90% of patients get an amoxicillin rash with EBV - 5% do with no EBV.
Viral Pharyngitis
Viral infection will often affect immunocompromised and elderly patients. You normally see a unilateral erythema with ulceration. The lesions are often mirrored in the distribution of the glossopharyngeal nerve.
CMV Tonsillitis
This presents very similarly to EBV, and if symptoms persist but the monospot remains negative it should be considered. There is a lot of fever and malaise.
HIV Tonsillitis
Uncommon but should be considered if there is no exudate, tonsillar hypertrophy, rash and mucocutaneous ulceration.
Globus Pharyngeus
This is painless, and patients complain of having "something in the throat", with symptoms improved by swallowing.
Agranulocytosis
Can present with a sore throat, and can be caused by a number of drugs, carbimazole in particular.
Quinsy - peritonsillar abscess
Full, erythematous appearance of the peritonsilar area.
-Deviation of the uvular
-Trismus
- Lateralising pain
- Fullness of the soft palate on the affected side
- Reduction in neck mobility
There is a risk of re-accumulation after drainage. There is no evidence for antibiotics after drainage, but they are generally given.
Quinsy can spread to the parapharyngeal abscess which can be fatal if not treated. Signs can be subtle, and underlying masses might not be fluctuant.
Treatment
Single doses of prednisolone or dexamethasone can be very helpful in major cases - in minor cases they decrease pain by six hours.
Despite their regular use, antibiotics are rarely indicated. Even the SIGN guidelines suggest we use CENTOR guidelines!
The Centor Score - sensitive 97% and specificity 78%
History of fever or temperature > 38oC +1
Absence of cough +1
Tender anterior cervical lymphadenopathy +1
Tonsillar swelling or exudates +1
Age ≥45 years -1
A score of 4-5 means that antibiotics should be prescribed.
Antibiotics should be given if there is an increased risk of complications - immuo-suppressed patients, history of valvular heart disease, history of rheumatic fever. If there is an outbreak of GABHS infection within an institution, and a history of repeated episodes of proven GABHS infection.
Streptococcal Score Card - for children
5 to 15 years
Season (late autumn, winter, early spring)
Fever (≥38.3°C)
Cervical lymphadenopathy
Pharyngeal erythema, oedema, or exudate
No symptoms of a viral upper respiratory infection (conjunctivitis, rhinorrhoea, or cough)
If 5 of the criteria are met, a positive culture for GABHS is predicted in 59% of children; if 6 of the criteria are met, a positive culture is predicted in 75% of children.
Tonsillectomy
Patients with seven attacks in one year, five in two consecutive years, or three attacks in three consecutive years warrant referral to an ENT department.
References
http://www.annemergmed.com/article/S0196-0644(13)00687-2/pdf
http://rebelem.com/patients-strep-throat-need-treated-antibiotics/
http://www.smartem.org/podcasts/treatment-acute-pharyngitis
http://radiopaedia.org/cases/tonsillitis
http://lifeinthefastlane.com/ent-equivocation-002/
http://www.ncbi.nlm.nih.gov/pubmed/?term=Hayward+G%2C+Thompson+MJ%2C+Perera+R%2C+et+al.+Corticosteroids+as+standalone+or+add-on+treatment+for+sore+throat.+Cochrane+Database+Syst+Rev.+2012%3B10%3ACD008268.+http%3A%2F%2Fdx.doi.org%2F10.1002%2F14651858.CD008268.pub2
http://learning.bmj.com/learning/module-intro/sore-throat-diagnostic-picture-tests.html?moduleId=6058292&searchTerm=%E2%80%9Cthroat%E2%80%9D&page=1&locale=en_GB
http://www.sign.ac.uk/guidelines/fulltext/117/index.html
http://www.rcemlearning.co.uk/modules/acute-sore-throat/
http://dontforgetthebubbles.com/tonsillitis/
http://www.rcemlearning.co.uk/references/acute-sore-throat/
http://www.rcemlearning.co.uk/modules/psor-throat/
http://www.rcemlearning.co.uk/modules/sore-throat-with-a-fruity-appearance/
http://www.rcemlearning.co.uk/modules/holiday-sore-throat-are-antibiotics-required/
http://www.aliem.com/modern-em-case-1-and-2-strep-throat/
http://www.aliem.com/paucis-verbis-card-strep-pharyngitis/
There could also be Lemierre's syndrome, retropharyngeal abscess, diptheria, bacterial tracheitis, Ludwig's angina or angioedema.
Red flags for sore throat including significant systemic upset, severe pain, stridor, severe neck stiffness, inability to swallow or tripod position.
Causes
Group A β haemolytic streptococcus - 5-15%
Can cause rheumatic fever in some patients, toxic shock syndrome, necrotising fascitis and post-strep glomerulonephritis. GABHS can be carried asymptomatically - mostly between 3 and 15yrs old (carriage rates 5 - 21%). Adults have much lower carriage rates.
Complications can be suppurative (otitis media, sinusitis, peritonsillar abscess) or non-suppurative (rheumatic fever).
Treat with pen V, 500mg QDS for 10 days.
Viral Tonsillitis
Tonsillitis/pharyngitis are: rhinovirus; coronavirus; adenovirus; herpes simplex; parainfluenza; echovirus; coxsackie A; Epstein-Barr; CMV.
Epstein-Barr Virus
This causes infectious mononucleosis which presents with malaise, headache, fever, pharyngitis, posterior cervical node enlargement, splenomegaly and hepatomegaly. There is a lethargy lasting for six to eight weeks, with suffers being infective for weeks to months. Glandular fever causes anterior and posterior chain lymphadenopathy - bacterial is normally just the upper anterior cervical chain.
Diagnosis is supported by monospot, and there may be atypical lymphocytes and deranged liver enzymes.
90% of patients get an amoxicillin rash with EBV - 5% do with no EBV.
Viral Pharyngitis
Viral infection will often affect immunocompromised and elderly patients. You normally see a unilateral erythema with ulceration. The lesions are often mirrored in the distribution of the glossopharyngeal nerve.
CMV Tonsillitis
This presents very similarly to EBV, and if symptoms persist but the monospot remains negative it should be considered. There is a lot of fever and malaise.
HIV Tonsillitis
Uncommon but should be considered if there is no exudate, tonsillar hypertrophy, rash and mucocutaneous ulceration.
Globus Pharyngeus
This is painless, and patients complain of having "something in the throat", with symptoms improved by swallowing.
Agranulocytosis
Can present with a sore throat, and can be caused by a number of drugs, carbimazole in particular.
Quinsy - peritonsillar abscess
Full, erythematous appearance of the peritonsilar area.
-Deviation of the uvular
-Trismus
- Lateralising pain
- Fullness of the soft palate on the affected side
- Reduction in neck mobility
There is a risk of re-accumulation after drainage. There is no evidence for antibiotics after drainage, but they are generally given.
Quinsy can spread to the parapharyngeal abscess which can be fatal if not treated. Signs can be subtle, and underlying masses might not be fluctuant.
Treatment
Single doses of prednisolone or dexamethasone can be very helpful in major cases - in minor cases they decrease pain by six hours.
Despite their regular use, antibiotics are rarely indicated. Even the SIGN guidelines suggest we use CENTOR guidelines!
The Centor Score - sensitive 97% and specificity 78%
History of fever or temperature > 38oC +1
Absence of cough +1
Tender anterior cervical lymphadenopathy +1
Tonsillar swelling or exudates +1
Age ≥45 years -1
A score of 4-5 means that antibiotics should be prescribed.
Antibiotics should be given if there is an increased risk of complications - immuo-suppressed patients, history of valvular heart disease, history of rheumatic fever. If there is an outbreak of GABHS infection within an institution, and a history of repeated episodes of proven GABHS infection.
Streptococcal Score Card - for children
5 to 15 years
Season (late autumn, winter, early spring)
Fever (≥38.3°C)
Cervical lymphadenopathy
Pharyngeal erythema, oedema, or exudate
No symptoms of a viral upper respiratory infection (conjunctivitis, rhinorrhoea, or cough)
If 5 of the criteria are met, a positive culture for GABHS is predicted in 59% of children; if 6 of the criteria are met, a positive culture is predicted in 75% of children.
Tonsillectomy
Patients with seven attacks in one year, five in two consecutive years, or three attacks in three consecutive years warrant referral to an ENT department.
References
http://www.annemergmed.com/article/S0196-0644(13)00687-2/pdf
http://rebelem.com/patients-strep-throat-need-treated-antibiotics/
http://www.smartem.org/podcasts/treatment-acute-pharyngitis
http://radiopaedia.org/cases/tonsillitis
http://lifeinthefastlane.com/ent-equivocation-002/
http://www.ncbi.nlm.nih.gov/pubmed/?term=Hayward+G%2C+Thompson+MJ%2C+Perera+R%2C+et+al.+Corticosteroids+as+standalone+or+add-on+treatment+for+sore+throat.+Cochrane+Database+Syst+Rev.+2012%3B10%3ACD008268.+http%3A%2F%2Fdx.doi.org%2F10.1002%2F14651858.CD008268.pub2
http://learning.bmj.com/learning/module-intro/sore-throat-diagnostic-picture-tests.html?moduleId=6058292&searchTerm=%E2%80%9Cthroat%E2%80%9D&page=1&locale=en_GB
http://www.sign.ac.uk/guidelines/fulltext/117/index.html
http://www.rcemlearning.co.uk/modules/acute-sore-throat/
http://dontforgetthebubbles.com/tonsillitis/
http://www.rcemlearning.co.uk/references/acute-sore-throat/
http://www.rcemlearning.co.uk/modules/psor-throat/
http://www.rcemlearning.co.uk/modules/sore-throat-with-a-fruity-appearance/
http://www.rcemlearning.co.uk/modules/holiday-sore-throat-are-antibiotics-required/
http://www.aliem.com/modern-em-case-1-and-2-strep-throat/
http://www.aliem.com/paucis-verbis-card-strep-pharyngitis/
Sunday 7 June 2015
e-FAST - Pneumothorax
We've talked about FAST...now we need to put the "E" into it. The E wasn't taught to me in my course, and isn't mentioned on the college e-learning module, but it is on their checklist to be assessed for competence...
How
- Ideally you need a linear probe
- Place the probe in the 2nd or 3rd IC space, midclavicular line, and slide caudally.
Bat Sign - the top rib looks like a bat flying out of the screen
- Then look in the 6th IC space, ant axillary line
Normal
Comet Tails - artifacts from the pleural line. Sliding lung and comet tails are normal.
Seashore Sign or waves on a sandy beach- normal lung sliding on M mode.
 - from http://www.intechopen.com/books/hot-topics-in-echocardiography/lung-ultrasound-comet-tails-technique-and-clinical-significance
- from http://www.intechopen.com/books/hot-topics-in-echocardiography/lung-ultrasound-comet-tails-technique-and-clinical-significance
 - from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
- from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
Pneumothorax
Loss of pleural sliding/ loss of the seashore sign in a spontaneously breathing patient.
This leads to the stratosphere or bar code sign.
No comet tails
 - from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
- from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
References
https://www.acep.org/Clinical---Practice-Management/Focus-On--EFAST---Extended-Focused-Assessment-With-Sonography-for-Trauma/
https://www.youtube.com/watch?v=Yg78aU93SZE
https://www.youtube.com/watch?v=EVQTI7ivhFM
https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
How
- Ideally you need a linear probe
- Place the probe in the 2nd or 3rd IC space, midclavicular line, and slide caudally.
Bat Sign - the top rib looks like a bat flying out of the screen
- Then look in the 6th IC space, ant axillary line
Normal
Comet Tails - artifacts from the pleural line. Sliding lung and comet tails are normal.
Seashore Sign or waves on a sandy beach- normal lung sliding on M mode.
 - from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
- from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/Pneumothorax
Loss of pleural sliding/ loss of the seashore sign in a spontaneously breathing patient.
This leads to the stratosphere or bar code sign.
No comet tails
 - from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
- from https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/References
https://www.acep.org/Clinical---Practice-Management/Focus-On--EFAST---Extended-Focused-Assessment-With-Sonography-for-Trauma/
https://www.youtube.com/watch?v=Yg78aU93SZE
https://www.youtube.com/watch?v=EVQTI7ivhFM
https://sonospot.wordpress.com/2012/06/19/sonoapp-lung-ultrasound-the-down-low-of-pneumo-with-the-help-of-lichtenstein-of-course/
Tuesday 14 April 2015
Myocarditis
- active viral
* coxsackie virus B - enterovirus
* parasitic - Chagas' disease is the most common cause. Endemic in Central and South America
- post viral (lymphocytic - or rheumatic fever)
- hypersensitivity
- autoimmune (SLE, polymyositis, scleroderma, sarcoidosis, DM, thyrotoxicosis, IBD)
- infectious
- giant cell myocarditis
- (HIV is normally another infection rather than being causative)
- Often with a prodrome of fever, malaise and arthralgia (89%)
- 60% have a fever, 15% have palpitations
- May be with myopericarditis.
May be quite hard to differentiate from ACS, especially with troponin rises.
Signs
Fever, tachycardia, pericardial rub + signs of failure.
Investigations
Cardiac biomarkers may be elevated - but only 1/2 of patients had an elevated troponin
ECG: non-specific ST segment and T wave changes. Sinus tachycardia. ECG changes not normally in single vessel territory.
CXR: Normal, or features of cardiomegaly
Echo: Let ventricular dysfunction in 69% of patients
Treatment
Supportive - inotropes if needed
Immunosuppressive therapy has no evidence.
Prognosis
Heart failure, syncope, BBB or reduced ejection fraction on echo all are associated with poor outcome.
References
Saturday 4 April 2015
Pulmonary Oedema
Pulmonary oedema - a sign of heart failure, not synonomous
Cardiac Causes:
Causes of Pulmonary Oedema
Left ventricle can't empty, causing raised pressure in the lungs. This means the hydrostatic pressure is greater than the oncotic pressure. Fluid moves into the interstitium and alveoli. Some of it is reabsorbed by the lymphatic system. If this can't happen, the accumulating fluid starts to hinder gas exchange, resulting in hypoxia.
The hypoxia triggers catecholamine release causing vasoconstriction and further left ventricle emptying problems.
#fcem #FOAMed #revision #cardiology Causes of acute cardiogenic pulmonary oedema. pic.twitter.com/7behCnlQzl
— Kirsty Challen (@KirstyChallen) July 23, 2013
Specifically left heart failure and mitral regurgitationNon Cardiac Causes: NOTCARDIAC or IS NOT THE HEART
#fcem #FOAMed #revision #respiratory Causes of non-cardiogenic pulmonary oedema. pic.twitter.com/Ou7HJUEAWP
— Kirsty Challen (@KirstyChallen) August 20, 2013
I nhaled Toxins (Ammonia, Chlorine, Phosgene, Nitrous oxide, heroin)S IRS / Sepsis / Septic Shock
N eurogenic (seizure, strangulation, trauma)
O verdose (Heroin, methadone, cocaine)
T hyrotoxicosis
T rauma
H eat (Smoke! Remember to also consider carbon monoxide!)
E lectrocution
H igh altitude pulmonary edema
E mbolism (Pulmonary Embolism, Acute Gas Embolism, Amniotic Fluid Embolism)
A spirin toxicity
R eperfusion or Re-expansion (ARDS)
T ransfusion
asthma, post-obstructive/ post intubation, near drowning
Neurogenic - pulmonary oedema after a significant CNS insult, probably as a result of a catecholamine surg. It's under recognised, and may happen after head injuries. Management is still supportive, and treat the underlying CNS insult.
Presentation
Typically mentioned acute dyspnoea with frothy blood stained sputum. Some of the more recent articles on pulmonary oedema have split the presentation into four categories, and this makes the management and the presentation make a lot more sense.
1. SCAPE - Sympathetic Crashing Acute Pulmonary (O)Edema)
Often there is no history of CCF, no oedema, no clear ‘trigger’, normal LV function. This process is largely neuro-hormonal in aetiology and comes on pretty quickly – over hours.
2. Acute-on-chronic (Acute decompensated HF)
Slower onset - over days
3. Acute Causes
These people have a new cause for their oedema - ACS / STEMI, rapid AF / arrhythmia, PE, valve rupture, high output state – sepsis, anaemia. Often a reversible cause.
4. Iatrogenic
Too much IV fluids to treat a chronically low blood pressure!
Clinical Examination
Bibasal inspiratory crepitations or wheeze.
Pale, cold and clammy
Sinus tachycardia or atrial fibrillation
Gallop rhythm may be present.
Murmurs, especially mitral regurgitation and aortic stenosis, may be a precipitating cause.
Assess the JVP, mucus membranes and urine output.
Look for peripheral oedema and hepatomegaly suggesting right heart failure.
Treatment
- CPAP
Lots of studies suggest the first thing you should do is put CPAP on. BiPAP instead doesn't cause harm - so only use it if there's hypercapnea too.
Start at 6 cmH20 and rapidly increase to 10cmH20 as tolerated.
The classic indications for CPAP are:
pH<7.35
RR >20/min
With "official cautions" being right ventricular failure, cardiogenic shock, severe obstructive airways disease, agitated patient. Contraindications are ET indicated, resp arrest, life threatening hypoxia, unconscious patient.
RR >20/min
With "official cautions" being right ventricular failure, cardiogenic shock, severe obstructive airways disease, agitated patient. Contraindications are ET indicated, resp arrest, life threatening hypoxia, unconscious patient.
- Nitrates
Help reduce afterload.
Resources seem to suggest a higher dose than I've ever used - 400mcg/ minute. As a GTN SL spray is 400mcg/dose, my assumption would be whilst you're mixing up the infusion, get SL in! Put a big bolus in initially to get the GTN up into the therapeutic range. Get an ART line in as soon as possible, so you can control the BP well.
Be really careful using nitrates in patients with aortic stenosis.
- Morphine
Morphine is associated with increased mortality, although it makes your patients feel better - so don't give it. They have a theoretical physiological advantage as they reduce pre-load, but this is not born out in real life.
- Diuretics
These have caused much controversy in the NICE guidelines. I've never much liked giving a big dose of furosemide as it takes so long to work - and a lot can happen whilst you're waiting, and it causes a lot of harm. Evidence now suggests that as some patients in pulmonary oedema are euvolaemic, they can make the patients worse.
Diuretics reduced preload (prevent NaCl reabsorption --> increased fluid excretion and vasodilate).
- Inotropes
Commence early, and stop early. Dobutamine - 2-3mcg/kg/min and increase as required.
Investigations
ECG - rarely normal. Often tachycardia, and possibly left ventricular hypertrophy.
May show precipitating causes - ST segment changes or arrhythmia
CXR -Excludes other causes
cardiogmegaly, interstitial and alveolar oedema and upper lobe diversion.
bat wing or butterfly shadowing - perihilar shadowing
peri-bronchial cuffing
pleural effusions
Kerley lines:
A lines - course towards hilar. Thickening of the interlobular septa. Only really seen on HRCT
B lines - 1-2 cm thin lines in the peripheries of the lung. Extend to pleural surface. Perpendicular to the pleural surface. Usually seen at lung bases.
C lines - short lines that do not reach the pleura
D lines - B lines seen on lateral CXRs
Differential is diffuse pulmonary haemorrhage - has no dependent gradient, and usually no pleural effusion.
ABG- Type 1 respiratory failure (hypoxaemia)
Bloods
Take FBC, U&E, LFT, troponin and INR to identify precipitants
Check BNP - produced by stretched cardiomyoctes. No limited identified for acute diagnosis, but BNP is sensitive so can rule out heart failure as a cause of breathlessness - unless the heart failure has happened very very quickly. It can also be raised in sepsis, renal or liver failure, hypoxia, myocardial ischaemia and tachycardia.
Prognosis
Worse outcome if:
Advanced Age
Wide QRS
Low LVF
Hypotension
Precipitated by ischaemia
Previous hospitalisation for heart failure
Marked BNP elevation
Elevated troponin
Hyponatraemia and raised urea and creatinine
References
http://lifeinthefastlane.com/ccc/negative-pressure-pulmonary-oedema/
http://emj.bmj.com/content/22/5/391.1.full
http://emlyceum.com/2011/07/25/acute-pulmonary-edema-answers/
http://boringem.org/2014/07/24/tiny-tips-non-cardiogenic-pulmonary-edema/
http://radiopaedia.org/cases/acute-pulmonary-oedema-1
http://radiopaedia.org/articles/septal-lines-in-lung
http://cdn.lifeinthefastlane.com/wp-content/uploads/2009/11/treatment-of-severe-heart-failu.pdf
http://crashingpatient.com/medical-surgical/cardiology/heart-failure-acute-pulmonary-edema.htm/
http://broomedocs.com/2011/04/clinical-case-004-post-op-peep/
http://broomedocs.com/2011/08/clinical-case-020-the-abc-of-apo/
http://lifeinthefastlane.com/oncology-quandary-004/
http://cdn.lifeinthefastlane.com/wp-content/uploads/2009/11/pulmonary-oedema.pdf
http://lifeinthefastlane.com/aftb-lecture-notes-acute-pulmonary-oedema/
http://lifeinthefastlane.com/ccc/neurogenic-pulmonary-oedema/
http://www.rcemlearning.co.uk/modules/cardiogenic-pulmonary-oedema/
http://www.rcemlearning.co.uk/references/cardiogenic-pulmonary-oedema/
http://lifeinthefastlane.com/ccc/severe-heart-failure-management/
http://radiopaedia.org/articles/pulmonary-oedema
http://www.rcemlearning.co.uk/modules/think-about-it/
http://lifeinthefastlane.com/ebm-acute-pulmonary-oedema/
http://boringem.org/2014/07/24/tiny-tips-non-cardiogenic-pulmonary-edema/
http://www.emdocs.net/furosemide-treatment-acute-pulmonary-edema/?utm_content=bufferc2fc4&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer#comments
http://radiopaedia.org/cases/apo-arrowsjpg
http://radiopaedia.org/articles/bat-wing-pulmonary-opacities-1
http://t.co/sZ7m5DbMTr
http://emtutorials.com/2013/10/killer-sausage/?utm_source=feedburner&utm_medium=email&utm_campaign=Feed%3A+EMTutorials+%28EM+Tutorials%29
http://calgaryguide.ucalgary.ca/Cardiology.aspx
http://lifeinthefastlane.com/book/critical-care-drugs/gtn-ntg/
Thursday 26 February 2015
FAST
I think I make FAST scanning more complicated than it needs to be. Four views - lungs are in eFAST, not FAST...although CEM has them on their checklist.
RUQ - Pouch of Rutherford-Morrison
- Start just anterior to the mid-axillary line, angled slightly backwards.
- Slide the probe towards the head to get a view of the diaphragm
- Look for pleural fluid - a jet black triange just above the diaphragm
- Ask the patient to take a deep breath if possible, particularly if rib shadows obscure the area of interest.
LUQ - Spleno-renal angle
- Posterior-axillary line at about the 6th to 9th intercostal space
- To get rid of rib shadows, and to get a better view of the spleen, slide the probe towarsd the hed and rotate it very slightly clockwise, producing an intercostal oblique view, so that the spleen (not the kidney) is seen.
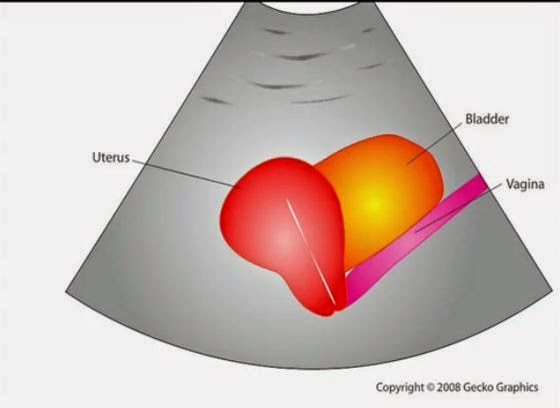
Pelvic - Pouch of Douglas in females, rectovesical pouch in male
Fluid will collect here.
Place the probe on the pubic bone and note a bone shadow. Slide slightly towards the head to get a good longitudinal pelvic view.
Full bladder will be triangular in shape.
In a female, the body of the uterus sits in the intraperitoneal space just posterior to the bladder (Figure 19), so free fluid will be seen just posterior to the uterus. This space is often called the pouch of Douglas and sometimes just small amounts can be detected
Cardiac
Subxiphoid view - probe laid almost flat and angled towards the head. Apply probe pressure to indent the epigastrium
Pitfalls
Perinephric fat, especially in obese patients, may be misinterpreted as intraperitoneal free fluid. Consider comparison views between each kidney.
Free fluid isn’t always blood; consider ascites, fluid related to a ruptured ovarian cyst, ruptured bladder or peritoneal dialysis.
90% sensitive and 99% specific for traumatic haemoperitoneum
References
Emergency Ultrasound Made Easy
http://www.trauma.org/index.php/main/article/214/
http://www.sonoguide.com/FAST.html
CEM Website
RUQ - Pouch of Rutherford-Morrison
- Start just anterior to the mid-axillary line, angled slightly backwards.
- Slide the probe towards the head to get a view of the diaphragm
- Look for pleural fluid - a jet black triange just above the diaphragm
- Ask the patient to take a deep breath if possible, particularly if rib shadows obscure the area of interest.
LUQ - Spleno-renal angle
- Posterior-axillary line at about the 6th to 9th intercostal space
- To get rid of rib shadows, and to get a better view of the spleen, slide the probe towarsd the hed and rotate it very slightly clockwise, producing an intercostal oblique view, so that the spleen (not the kidney) is seen.
Pelvic - Pouch of Douglas in females, rectovesical pouch in male
Fluid will collect here.
Place the probe on the pubic bone and note a bone shadow. Slide slightly towards the head to get a good longitudinal pelvic view.
Full bladder will be triangular in shape.
In a female, the body of the uterus sits in the intraperitoneal space just posterior to the bladder (Figure 19), so free fluid will be seen just posterior to the uterus. This space is often called the pouch of Douglas and sometimes just small amounts can be detected
Cardiac
Subxiphoid view - probe laid almost flat and angled towards the head. Apply probe pressure to indent the epigastrium
Pitfalls
Perinephric fat, especially in obese patients, may be misinterpreted as intraperitoneal free fluid. Consider comparison views between each kidney.
Free fluid isn’t always blood; consider ascites, fluid related to a ruptured ovarian cyst, ruptured bladder or peritoneal dialysis.
90% sensitive and 99% specific for traumatic haemoperitoneum
References
Emergency Ultrasound Made Easy
http://www.trauma.org/index.php/main/article/214/
http://www.sonoguide.com/FAST.html
CEM Website
Monday 16 February 2015
Carbon Monoxide
I thought I knew about Carbon Monoxide poisoning, and then I went to an (R)CEM day - and learnt a whole lot more about it.
Numbers
4,000 attend ED with CO
200 hospitalised
50 die each year
Pathophysiology
CO binds to haemoglobin with an affinity of approximately 220 times that of oxygen. CO shifts the oxygen dissociation curve to the left. It also binds to myoglobin and mitochondrial cytochrome oxidase, impairing ATP production. Somehow it also binds to platelets so that nitric oxide gets released.
CO binds to fetal haemoglobin and shifts the already left-shifted fetal oxyhaemoglobin dissociation curve further to the left. The half-life of CO in the fetus is longer than in the Mum.
Numbers
4,000 attend ED with CO
200 hospitalised
50 die each year
Pathophysiology
CO binds to haemoglobin with an affinity of approximately 220 times that of oxygen. CO shifts the oxygen dissociation curve to the left. It also binds to myoglobin and mitochondrial cytochrome oxidase, impairing ATP production. Somehow it also binds to platelets so that nitric oxide gets released.
CO binds to fetal haemoglobin and shifts the already left-shifted fetal oxyhaemoglobin dissociation curve further to the left. The half-life of CO in the fetus is longer than in the Mum.
CO is produced continuously in the body as a by-product of haem breakdown. This leads to a normal baseline COHb concentration of about 0.5%. In pregnancy and haemolytic anaemias this can rise towards 5%.
Animal research – dogs given COHb 65-70%. They died.
2/3 of blood removed, and replaced with already poisoned blood - they were fine. They were then injected with CO, and were also fine.
- Cigarette smoking leads to COHb concentrations of up to about 12% in heavy smokers
Non-smokers living away from urban areas have carboxyhaemoglobin concentrations of between 0.4% and 1.0%.
In an urban or industrial setting, concentrations of up to 5% may be considered normal.
- Methylene chloride (dichloromethane), which is found in some paint strippers and sprays. Once in the liver, is converted to carbon monoxide. Methylene chloride is stored in body tissues and released gradually.
- Electric fires, fires, wood burning stoves, barbeques, shesha pipes gas - anything.
Clinical Presentation
With prolonged exposure her symptoms could lead to hypotension, seizures, cerebral oedema, metabolic acidosis and respiratory failure.
4.3% of 1758 patients presenting to 4 EDs had raised COHb levels
Unsuspected positive cases 3.5%:
COPD 7.5%
Headache 6.3%
Flu-like 4.3%
Chest pain 3.3%
Seizures 2.1%
More Severe Symptoms:
The appearance of intoxication or a personality change
Impaired mini mental-state examination
Vertigo and ataxia
Breathlessness and tachycardia
Chest pain (due to angina or myocardial infarction)
Loss of consciousness
Seizure or multiple seizures
Abnormal neurological signs including blindness, deafness, and extrapyramidal effects.
High risk features include chest pain, history of unconsciousness, any continuing neurological symptoms or signs (especially cerebellar features) and pregnancy due to the effects on the foetus
Chronic Presentation
Chronic fatigue
Emotional distress
Memory deficits
Difficulty concentrating
Sleep disturbances
Vertigo
Neuropathy
Paraesthesias
Recurrent infection
Polycythaemia
Abdominal pain
Diarrhoea
Clinical Assessment
Neuro exam: including tests of coordination and balance, MMSE, short term memory for chronic.
Cherry red skin is only seen in severe poisoning, with levels >20.
Investigations
CO reading taken from a breath analyzer - lactose intolerant patients have raised H2 in their expired breath which can interfere with the readings.
Venous blood should be taken into anti-coagulant and sent to the laboratory.
Treatment
Administration of oxygen speeds the elimination of CO from the body. Without therapy, the elimination half life of CO is 4-6 hours. Administration of high flow oxygen by a tight fitting mask at normal atmospheric pressure reduces half life to approximately 76 mins.
Get your NIV out – you just need the seal and the flow rates of O2 high enough to maintain 100% oxygen. Even manually holding a BVM over them with a good seal does the job.
There is debate about the added value provided by hyperbaric oxygen. A COHb concentration of >20% should be an indication to consider hyperbaric oxygen especially if has any other symptoms:
Loss of consciousness at any stage
Neurological signs other than headache
Myocardial ischaemia/arrhythmia diagnosed by ECG
The patient is pregnant
If metabolic acidosis persists despite correction of hypoxia and adequate fluid resuscitation consider correction with intravenous sodium bicarbonate.
I wrote a powerpoint presentation on this - ages ago - feel free to use and adjust...
References
Toxbase
Tuesday 10 February 2015
Cyanide
There was a chemical incident declared once because the pre-hospital team could smell almonds- they thought cyanide could be involved. Turns out someone had been baking...
Cyanide is released by the incomplete combustion of nitrogen-containing materials, and metabolised from amygdalin. Amygdalin can be found in the pits of many fruits, such as apricots and papayas and raw nuts.
Cyanide is a colourless gas with a bitter almond smell, detectable by only 40% of people.
 |
| http://www.christem.com/storage/cyanide%20mechanism |
Symptoms
#fcem #toxicology #FOAMed #revision Features of cyanide toxicity. pic.twitter.com/1UYxjDrIPI
— Kirsty Challen (@KirstyChallen) July 15, 2014
Symptoms after exposure to high vapor concentrations may include the following:Transient hyperpnea and hypertension 15 seconds after inhalation
Loss of consciousness in 30 seconds
Respiratory arrest in 3-5 minutes
Bradycardia, hypotension, and cardiac arrest within 5-8 minutes of exposure
Symptoms after exposure to lower vapor concentrations or after ingestion or liquid exposure may include the following:
Feelings of apprehension or anxiety
Vertigo
Nausea, with or without vomiting
Muscular trembling
Loss of consciousness
Headache
Dyspnea
Patients exposed to cyanogen chloride experience severe eye and mucous membrane irritation.Low-dose exposure results in rhinorrhea, bronchorrhea, and lacrimation. Inhalational exposure results in dyspnea, cough, and chest discomfort. Onset of symptoms after exposure to nitriles (acetonitrile and/or propionitrile) may be significantly delayed.
Physical findings of cyanide exposure are generally nonspecific. They classically have cherry red skin.
Laboratory Investigations
- Normal arterial oxygen tension, high venous oxygen tension = decreased AV difference (<10%)
- High anion gap metabolic acidosis
- Raised lactate
Antidotes
#REBELReview 67 Cyanide Toxicity Treatment http://t.co/Fo3oz5PIN2 #FOAMed #FOAMtox #MedEd #ABIM #EMBoardReview #USMLE pic.twitter.com/j6FlhcmlKs
— Salim R. Rezaie (@srrezaie) June 1, 2014
To accompany episode # 1.. a fabulous #FOAMed visual representation of the mech of action of cyanide antidotes http://t.co/RxRCsTmnci
— FOAMcast (@FOAMpodcast) May 24, 2014
Minimal symptoms that resolve spontaneously need observation only.Other Factors
- Oxygen
- Consider sodium bicarbonate if severe lactic acidosis
- Treat haemodynamic instability and cerebral oedema
@Lmellick video on smoke inhalation injury https://t.co/SbhSGXZWZX #FOAMed
— Jasmin Hamzic (@jasmin_hamzic) January 11, 2015
#EMSqoD A:Cyanide can be the toxic agent in smoke. http://t.co/r2Hu7eFs & http://t.co/Tt439mpi So use cyanokit, 50% increase in ROSC #FOAMed
— Dr. Howie Mell (@DrHowieMell) January 4, 2013
Cyanide poisoning: key facts
#FOAMed #Toxicology #FCEM pic.twitter.com/LYGWeNf451
— Natalie May (@_NMay) July 9, 2013
References
http://blog.clinicalmonster.com/2015/02/em-ccm-carbon-monoxide-and-cyanide-poisoning/
https://umem.org/educational_pearls/2675/
http://www.enlightenme.org/knowledge-bank/cempaedia/industrial-chemical-incidents
Friday 6 February 2015
Inhalation
The CEM syllabus says knows the rarer causes of breathless-ness including "inhalational injury from chemical and physical irritants, foreign body inhalation". A search for that came up with cyanide poisoning and methaemoglobinaemia - so have written a bit about them too on further blog posts. I also think that carbon monoxide poisoning is important - blog post to follow.
History
The following key points should be taken in a focused history
Exactly what exposed to and how much (ie volume and concentration)?
What route?
What protective measures were taken?
What treatment was given?
PPE
Some chemicals do not cause secondary contamination e.g. chlorine.
Smoke Inhalation
- Monitor for 4-6 hours in the ED.
- Observe for longer if high risk items in their history:
History of closed-space exposure for longer than 10 minutes
Carbonaceous sputum production
Arterial PO2 less than 60 mm Hg
Metabolic acidosis
Carboxyhemoglobin levels above 15%
Arteriovenous oxygen difference (on 100% oxygen) greater than 100 mm Hg
Bronchospasm
Odynophagia
Central facial burns
Pulmonary injury from smoke inhalation causes hyperinflation and atelectasis. Debris from cellular necrosis, inflammatory exudate, and shed epithelium combine with carbonaceous material to narrow airways that are already compromised by oedema. Reflex bronchoconstriction further worsens the obstruction.
Metals
Metal fume fever (MFF) is an acute disease induced by intense inhalation of metal oxides- mostly zinc. It is a self-limited syndrome characterized by fever, myalgias, headache, and nausea. Symptoms develop 4-12 hours after exposure and typically last several hours; severe cases generally resolve in 1-2 days. Observation is usually all that is necessary.
The exact pathology of MFF is not well understood but likely involves the deposition of fine metal particulates in the alveoli.
http://www.enlightenme.org/knowledge-bank/cempaedia/industrial-chemical-incidents
http://www.toxlearning.co.uk/course/view.php?id=21
http://emedicine.medscape.com/article/771194-overview
http://emedicine.medscape.com/article/814287-overview
http://emedicine.medscape.com/article/1005903-overview
http://emedicine.medscape.com/article/204178-overview#a0101
http://www.annemergmed.com/article/S0196-0644(05)80424-X/abstract
http://lifeinthefastlane.com/ccc/smoke-inhalation/
http://lifeinthefastlane.com/condom-inhalation/
http://lifeinthefastlane.com/toxicology-conundrum-038/
History
The following key points should be taken in a focused history
Exactly what exposed to and how much (ie volume and concentration)?
What route?
What protective measures were taken?
What treatment was given?
PPE
Some chemicals do not cause secondary contamination e.g. chlorine.
Smoke Inhalation
- Monitor for 4-6 hours in the ED.
- Observe for longer if high risk items in their history:
History of closed-space exposure for longer than 10 minutes
Carbonaceous sputum production
Arterial PO2 less than 60 mm Hg
Metabolic acidosis
Carboxyhemoglobin levels above 15%
Arteriovenous oxygen difference (on 100% oxygen) greater than 100 mm Hg
Bronchospasm
Odynophagia
Central facial burns
Pulmonary injury from smoke inhalation causes hyperinflation and atelectasis. Debris from cellular necrosis, inflammatory exudate, and shed epithelium combine with carbonaceous material to narrow airways that are already compromised by oedema. Reflex bronchoconstriction further worsens the obstruction.
Metals
Metal fume fever (MFF) is an acute disease induced by intense inhalation of metal oxides- mostly zinc. It is a self-limited syndrome characterized by fever, myalgias, headache, and nausea. Symptoms develop 4-12 hours after exposure and typically last several hours; severe cases generally resolve in 1-2 days. Observation is usually all that is necessary.
The exact pathology of MFF is not well understood but likely involves the deposition of fine metal particulates in the alveoli.
@Lmellick video on smoke inhalation injury https://t.co/SbhSGXZWZX #FOAMed
— Jasmin Hamzic (@jasmin_hamzic) January 11, 2015
http://www.enlightenme.org/knowledge-bank/cempaedia/industrial-chemical-incidents
http://www.toxlearning.co.uk/course/view.php?id=21
http://emedicine.medscape.com/article/771194-overview
http://emedicine.medscape.com/article/814287-overview
http://emedicine.medscape.com/article/1005903-overview
http://emedicine.medscape.com/article/204178-overview#a0101
http://www.annemergmed.com/article/S0196-0644(05)80424-X/abstract
http://lifeinthefastlane.com/ccc/smoke-inhalation/
http://lifeinthefastlane.com/condom-inhalation/
http://lifeinthefastlane.com/toxicology-conundrum-038/
Tuesday 27 January 2015
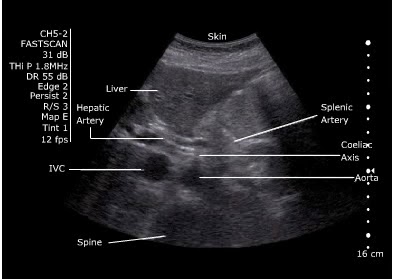
Abdominal Aorta Ultrasound
I'm rubbish at aorta ultrasounding, and it's one of the few scans that might actually be useful in the ED. I've done my level one course...but it was a while ago, and honestly...I can't remember what I'm looking for anymore. I've written this to try and remind myself...
This is assessed in the ultrasound level one course from CEM, with triggered assessments here.
This is assessed in the ultrasound level one course from CEM, with triggered assessments here.
Anatomy
Xiphoid, through until umbilicus (fourth lumbar vertebra)
- Coeliac axis is 1-2 cm below the diaphragm
- Superior mesenteric artery is 2 cm below the coeliac axis
- Inferior mesenteric artery is 4 cm above the bifurcation
Diameter - <2cm = normal, 2-3cm dilated but not aneurysmal, >3cm aneurysmal
Sens and Spec
Sensitivity of 96.3 % (95 % confidence interval (CI), 81.0 % to 99.9 %)
Specificity of 100 % (95 % CI, 91.8 % to 100 %)
Negative predictive value of 98.6 % (95 % CI, 88.0 % to 99.9 %)
Positive predictive value of 100 % (95 % CI, 86.8 % to 100 %)
Environment
Supine if possible
Curved probe.
Technique
- Start underneath the xiphisternum and identify the aorta - look for the vertebral body just behind it, liver anteriorly and bowel to the right.
- Make sure you are not looking at the IVC.
IVC: Right side, thin walled, compressible, transmitted pulse (‘double bounce’), almond shaped, shape varies
Aorta: left side, thick walled, will not compress, pulsatile, round in shape, constant shape
- Look for the coeliac axis. This is high and often difficult to see. It divides into splenic and hepatic artery - said to resemble the wings of a seagull. This is not essential to find.
- Sweep to the umbilicus
- Move the probe longitudionally and scan.
- Look for the "snowman" - where the SMA comes off at the coeliac trunk
Measure
Outer wall to outer wall.
No oblique or angled cuts
Problem Solving- Bowel Gas
“Jiggle” the probe, while applying gentle pressure.
Reposition the patient.
Try imaging from below the umbilicus with the probe directed cephalad.
Try imaging the aortic bifurcation from an oblique angle with the probe placed lateral to the umbilicus (right or left)
References
Subscribe to:
Posts (Atom)