This is assessed in the ultrasound level one course from CEM, with triggered assessments here.
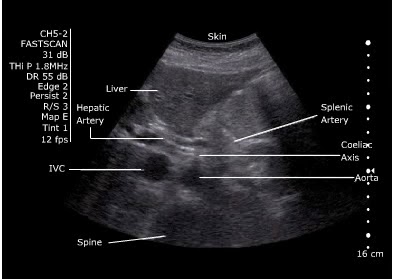
Anatomy
Xiphoid, through until umbilicus (fourth lumbar vertebra)
- Coeliac axis is 1-2 cm below the diaphragm
- Superior mesenteric artery is 2 cm below the coeliac axis
- Inferior mesenteric artery is 4 cm above the bifurcation
Diameter - <2cm = normal, 2-3cm dilated but not aneurysmal, >3cm aneurysmal
Sens and Spec
Sensitivity of 96.3 % (95 % confidence interval (CI), 81.0 % to 99.9 %)
Specificity of 100 % (95 % CI, 91.8 % to 100 %)
Negative predictive value of 98.6 % (95 % CI, 88.0 % to 99.9 %)
Positive predictive value of 100 % (95 % CI, 86.8 % to 100 %)
Environment
Supine if possible
Curved probe.
Technique
- Start underneath the xiphisternum and identify the aorta - look for the vertebral body just behind it, liver anteriorly and bowel to the right.
- Make sure you are not looking at the IVC.
IVC: Right side, thin walled, compressible, transmitted pulse (‘double bounce’), almond shaped, shape varies
Aorta: left side, thick walled, will not compress, pulsatile, round in shape, constant shape
- Look for the coeliac axis. This is high and often difficult to see. It divides into splenic and hepatic artery - said to resemble the wings of a seagull. This is not essential to find.
- Sweep to the umbilicus
- Move the probe longitudionally and scan.
- Look for the "snowman" - where the SMA comes off at the coeliac trunk
Measure
Outer wall to outer wall.
No oblique or angled cuts
Problem Solving- Bowel Gas
“Jiggle” the probe, while applying gentle pressure.
Reposition the patient.
Try imaging from below the umbilicus with the probe directed cephalad.
Try imaging the aortic bifurcation from an oblique angle with the probe placed lateral to the umbilicus (right or left)
References