GPs should be able to manage most asthma. The following points may be beneficial:
Steroids and "New" Drugs
Relvar Ellipta (GSK) is a dry powder inhaler that contains a corticosteroid (fluticasone furoate) and a long-acting beta2 agonist (vilanterol trifenatate). It is licensed for once-daily use as maintenance therapy for COPD and asthma.
Flixotide Evohaler is only available for the over 4s and Budesonide Easihaler only for those over 6. Seretide (fluticasone and serevent) is only for use in over 4s and Symbicort (budesonide and formoterol) only for the over 6s.
Methotrexate at low doses retains anti-inflammatory properties with little toxicity. In chronic severe asthma a number of mixed results have been reported with oral methotrexate.
Clinical issues
General questions, such as “how is your asthma today?” yield a non-specific answer; “I am ok”. Using closed questions, such as “do you use your blue inhaler every day?”, is likely to yield more useful information.
Education is a process and not a single event.
No patient should leave hospital without a written personalised asthma action plan.
Education should include personalised discussion of issues such as trigger avoidance and achieving a smoke-free environment to support people and their families living with asthma.
Brief simple education linked to patient goals is most likely to be acceptable to patients.
Do not recommend house dust mite avoidance to prevention asthma, or pet avoidance.
Treatment of reflux has no benefit in asthma control, although it does reduce dry cough.
Spacers
Single actuations of the metered dose inhaler into the spacer, each followed by inhalation.
Minimal delay between pMDI actuation and inhalation.
Tidal breathing is as effective as single breaths.
Spacers should be cleaned monthly rather than weekly as per manufacturer’s recommendations or performance is adversely affected. They should be washed in detergent and allowed to dry in air. The mouthpiece should be wiped clean of detergent before use.
Plastic spacers should be replaced at least every 12 months
References
http://bestbets.org/bets/bet.php?id=1768
Critical Care and Resuscitation 2005; 7: 119-127
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD007524.pub3/abstract
http://www.enlightenme.org/knowledge-bank/cempaedia/asthma-adults
http://www.enlightenme.org/the-curriculum-zone/node/2734
http://www.enlightenme.org/knowledge-bank/journal-scan/3mg-trial-randomised-trial-intravenous-or-nebulised-magnesium-sulphate-v
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002308.pub2/abstract
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002178/abstract
http://www.enlightenme.org/knowledge-bank/cem-ctr/acute-asthma-does-addition-magnesium-sulphate-have-clinically-significant-eff
http://www.enlightenme.org/learning-zone/acute-severe-wheeze-please
http://www.enlightenme.org/the-curriculum-zone/node/3771
http://www.enlightenme.org/knowledge-bank/cempaedia/breathlessness
http://www.aliem.com/lactic-acidosis-beta-agonist-therapy-asthma/
http://learning.bmj.com/learning/course-intro/asthmatic-patient.html?courseId=10046989&locale=en_GB = DONE
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002316.pub2/abstract
http://r1.emsworld.com/files/cygnus/image/EMSR/2011/AUG/640x360/pocketguide_patient_10342321.jpg
http://learning.bmj.com/learning/module-intro/quick-tips-asthma.html?moduleId=10050019&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/.html?moduleId=10051335&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/module-intro/occupational-asthma-evidence-based-diagnosis-management.html?moduleId=6051298&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://learning.bmj.com/learning/modules/flow/MCQ.html?execution=e9s1&moduleId=10029655&status=LIVE&action=start&_flowId=MCQ&sessionTimeoutInMin=90&locale=en_GB
http://www.enlightenme.org/knowledge-bank/cempaedia/asthma-adults
http://www.enlightenme.org/the-curriculum-zone/node/2734
http://learning.bmj.com/learning/course-intro/asthmatic%20patient.html?courseId=10046989&searchTerm=%E2%80%9Casthma%E2%80%9D&page=1&locale=en_GB
http://dontforgetthebubbles.com/emergency-medicine-clinical-excellence-series-pem-2-allergy-anaphylaxis-children/
http://www.enlightenme.org/knowledge-bank/cem-ctr/acute-asthma-does-addition-magnesium-sulphate-have-clinically-significant-eff
http://www.enlightenme.org/knowledge-bank/journal-scan/3mg-trial-randomised-trial-intravenous-or-nebulised-magnesium-sulphate-v
http://www.enlightenme.org/learning-zone/acute-severe-wheeze-please
http://ccforum.com/content/6/1/30
http://radiopaedia.org/articles/peri-bronchial-cuffing-2
http://radiopaedia.org/articles/asthma-1
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Findings%20on%20Investigations.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Clinical%20Findings.jpg
http://calgaryguide.ucalgary.ca/slide.aspx?slide=Asthma%20-%20Pathogenesis.jpg
https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2014/
https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-quick-reference-guide-2014/
Tuesday, 11 November 2014
Asthma - treatment
Moderate Severity Asthma Exacerbation
- 4 puffs salbutamol via a spacer, followed by 2 puffs every 2 minutes up to a maximum of 10 puffs
- Nebulisers if no spacer available or if the patient can't use it effectively.
Severe Acute Asthma
Steroids: Inhaled corticosteroids in the acute attack can help reduce hospitalisation. Little evidence that on discharge they improve things. Corticosteroids within an hour also help
Nebulisers: Allow concurrent oxygen administration.
A nebuliser takes 15-30 minutes to fully administer the drug. Administering more than 10mg of salbutamol per hour is unlikely to improve effectiveness but may increase side effects, which include tremor and tachycardia. Special delivery systems can deliver “continuous” nebulisers at 10mg per hour but are not usually available in the ED.
There is no evidence that 5mg nebulisers are superior to 2.5mg nebulisers.
Inhaled salbutamol can cause a lactic acidosis, worsening respiratory symptoms.
Salbutamol: No superiority of IV salbutamol over acute asthma. Systemic salbutamol has metabolic effects that may worsen respiratory function in asthma.
May be helpful if drug not delivered effectively (patient pulling mask off/ poor air entry).
Adrenaline: Nebulised adrenaline has shown no superiority and is a less selective agonist.
Anticholinergic: advocated in cases which are severe, life-threatening, or poorly responsive to ß2 agonist therapy.
Magnesium: Nebulised MgSO4 has no role
Limited role for intravenous MgSO4
Aminophylline: 5mg/kg over 20minutes loading dose
0.6mg/kg/hour IV infusion
If the patient is on maintenance take a baseline theophylline/ aminophylline level before maintenance infusion.
Furosemide: A theoretical bronchodilator of research interest, not better than nebulised ß2 agonists.
Rapid Sequence Induction
Use at least a size 8.0 diameter
Ketamine --> 1-2mg/kg helps bronchodilate
Avoid atracurium
Disconnect circuit during CPR to allow chest to deflate
Bilateral thoracostomies.
Discharge
Steroids if PEFR initially <50% best or predicted.
Stop abruptly after five days as long as patient continues on inhaled steroids.
Careful discharging patients that present late in the evening or early hours of the morning since the airways are naturally at their narrowest at around 4am.
When any of the following features are present, admission may be appropriate:
Referral if:
Two courses of systemic corticosteroids in the past year
- 4 puffs salbutamol via a spacer, followed by 2 puffs every 2 minutes up to a maximum of 10 puffs
- Nebulisers if no spacer available or if the patient can't use it effectively.
Severe Acute Asthma
Early steroid administration in acute severe asthmatic exacerbations is associated with a reduced need for hospital admission.
Steroids: Inhaled corticosteroids in the acute attack can help reduce hospitalisation. Little evidence that on discharge they improve things. Corticosteroids within an hour also help
A nebuliser takes 15-30 minutes to fully administer the drug. Administering more than 10mg of salbutamol per hour is unlikely to improve effectiveness but may increase side effects, which include tremor and tachycardia. Special delivery systems can deliver “continuous” nebulisers at 10mg per hour but are not usually available in the ED.
There is no evidence that 5mg nebulisers are superior to 2.5mg nebulisers.
Inhaled salbutamol can cause a lactic acidosis, worsening respiratory symptoms.
Salbutamol: No superiority of IV salbutamol over acute asthma. Systemic salbutamol has metabolic effects that may worsen respiratory function in asthma.
May be helpful if drug not delivered effectively (patient pulling mask off/ poor air entry).
Adrenaline: Nebulised adrenaline has shown no superiority and is a less selective agonist.
Anticholinergic: advocated in cases which are severe, life-threatening, or poorly responsive to ß2 agonist therapy.
Magnesium: Nebulised MgSO4 has no role
Limited role for intravenous MgSO4
2 g Magnesium Sulphate in 100 mls of normal saline given intravenously over 20 minutes
Aminophylline: 5mg/kg over 20minutes loading dose
0.6mg/kg/hour IV infusion
If the patient is on maintenance take a baseline theophylline/ aminophylline level before maintenance infusion.
Furosemide: A theoretical bronchodilator of research interest, not better than nebulised ß2 agonists.
NIV:
There is limited evidence for NIV. This is not currently supported by the British Thoracic Society. The patient must be supervised by the intensivist that can proceed immediately to intubation.
There is limited evidence for NIV. This is not currently supported by the British Thoracic Society. The patient must be supervised by the intensivist that can proceed immediately to intubation.
Rapid Sequence Induction
Use at least a size 8.0 diameter
Ketamine --> 1-2mg/kg helps bronchodilate
Avoid atracurium
Disconnect circuit during CPR to allow chest to deflate
Bilateral thoracostomies.
Discharge
Non-pharmacological management:
Advise parents with asthma about the the dangers to their children of smoking.
Weight loss and breathing exercise programmes can help with asthma symptoms
Inhalers
Check technique
GP follow up within two working days of treatment
Steroids if PEFR initially <50% best or predicted.
Stop abruptly after five days as long as patient continues on inhaled steroids.
Careful discharging patients that present late in the evening or early hours of the morning since the airways are naturally at their narrowest at around 4am.
The British asthma guideline discourages routine antibiotic prescription in acute asthma. Infective triggers are most commonly viral.
Patients considered for discharge should meet all of the following criteria:
No life-threatening features at any point (including pre-hospital)
No features of severe asthma after initial treatment
PEFR >75% best or predicted and stable one hour after initial treatment
or
PEFR >50% best or predicted and stable two hours after initial treatment
Still have significant symptoms
Concern over compliance
Lives alone
Psychosocial problems
Physical disability or learning difficulties
History of severe asthma
Presentation at night
Pregnancy
Exacerbation despite adequate dose steroids pre-presentation
Two courses of systemic corticosteroids in the past year
Two or more attendances at the ED for their asthma in the past year
On step 4 or 5 of the BTS/SIGN guidelines treatment ladder
Who has childhood asthma with concurrent food allergy
Deaths
There's a national review of asthma deaths (NRAD). All deaths where asthma is on the death certificate at all need to be reported.
Tuesday, 4 November 2014
Asthma - Pathophysiology and Clinical Signs
Asthma is really common and affects lots of people. It also causes lots of unnecessary deaths, and a lot of hospital attendances from asthma attacks. The 2014 asthma guidelines replace the word "exacerbation" with "attack" as it's easier to understand.
References for this summary will be at the end of part two.
Physiology


Asthma is defined as a chronic airway inflammatory disorder with airway hyper-responsiveness.
Asthma is an obstructive lung condition, caused essentially by an allergic reaction to a trigger. Like most reactions, there is exposure that sensitizes the helper T cells, then IgE is produced, mast cells - and then you get the response on the second and subsequent exposure. The release of histamines and leukotrienes causes vasodilation, increased mucus secretion and bronchial smooth muscles contraction. The reaction also causes eosinophils to migrate into the airways, eyes and nose causing conjunctivitis, rhinitis and bronchiole constriction.
Clinical Features

The Calgary Guide has a nice summary here. There's no thing that says with 100% certainty that this is asthma.
These features increase the probability of asthma:
- >1 of wheeze, cough, difficulty breathing, chest tightness
- particularly if the symptoms:
are worse at night/early morning
occur in response to exercise, allergen exposure or cold air
are triggered by aspirin or beta-blockers
occur in the absence of a cold
- Personal or family history of atopic disorder or asthma
- Widespread wheeze on chest auscultation
- Otherwise unexplained low FEV1 or PEFR
- Otherwise unexplained peripheral blood eosinophilia
These features lower the probability of asthma:
- Symptoms with colds only
- Chronic productive cough without wheeze or breathlessness
- Dizzyness, light-headedness or paraesthesia peripherally
- Voice disturbance
- Cardiac disease
- Significant smoking history (>20 pack years)
- Repeated normal chest examination when symptomatic
- Repeatedly normal PEFR or spirometry when symptomatic
Grading Systems
The SIGN (and British Thoracic Society) guidelines use clinical symptoms to grade the severity of an attack in adults and children. The NICE guidelines appear to be based on the SIGN guidelines.
Systolic paradox (pulsus paradoxus), an historical marker of severity of asthma, is unhelpful and wastes valuable time so has been removed from the guidelines.
Features of patients at high risk of a life-threatening asthma attack:
Using a short-acting beta agonist inhaler more than once every four hours
Using more than one short-acting bronchodilator inhaler per month
Fewer than 12 prescriptions for preventer medication in the past year
Concurrent mental health problems
Investigations
Normally a clinical diagnosis, but if the patient has an intermediate probability of asthma, investigations can help. The Calgary guide has a summary.
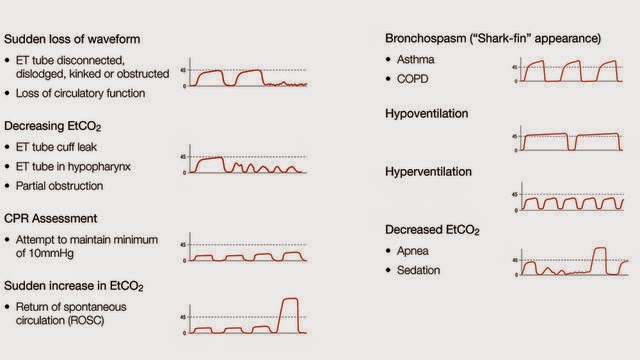
Capnography:
Wave form capnography should be used in acute exacerbations. Asthmatics get a "shark's fin" appearance because of the broncho-constriction.
Spirometry:
Spirometry shows reversibility and FEV1/FVC <0.7:
A decrease in FEV1 of > 15% after six minutes of exercise, or
An increase in FEV1 of > 15% after a two week trial of oral steroids (30 mg prednisolone once
daily), or
An increase in FEV1 of > 15% following therapy with a short acting beta 2 agonist
You can calculate the percentage change in FEV1 by:
Subtract the pre-bronchodilator FEV1 from the post-bronchodilator FEV1
Divide this by the pre-bronchodilator FEV1
Multiply by 100.
Peak Flow
60l/min. increase in PEFR) in response to either of the following strongly suggests underlying asthma:
400 mcg inhaled salbutamol
6-week trial of steroid inhaler (beclometasone 200 mcg bd or equivalent)
CXR
- Normal in up to 75% of patients
- pulmonary hyperinflation
- bronchial wall thickening - peribronchial cuffing
(non specific finding but may be present in ~48% of cases with asthma)
- pulmonary oedema due to asthma
CT
To look for complicated associated conditions such as allergic bronchopulmonary aspergillosis and not to directly diagnose asthma.
Non specific:
- bronchial wall thickening
- expiratory air trapping
- inspiratory decreased lung attenuation
- small centrilobular opacifities
- bronchial luminal narrowing - reduced
- bronchoarterial-diameter ratio
- sub segmental bronchiectasis - may be present in ~28-62% of asthmatics
Mimics
• Churg-Strauss
Look for signs and symptoms of systemic vasculitis, such as fever, weight loss, fatigue, and malaise, Be suspicious if there is a persistent eosinophilia, positive ANCA, and multiorgan involvement.
• COPD
• Anaphylaxis
4% of asthma admissions to PICU almost certainly had anaphylaxis rather than asthma - so make sure you consider it.
• Rhinitis
Management of chronic rhinosinusitis improves asthma control.
• Gastro-oesophageal reflux
Consider a three month trial of PPIs, as investigations to formally diagnose this are very invasive.
• Inhaled foreign body
• Airway stenosis
• Bronchiectasis
• Sarcoidosis
• Lung cancer
• Obliterative bronchioloitis
• Congestive cardiac
failure
• Pulmonary embolus
• Pulmonary fibrosis
• Hyperventilation syndrome
• Chronic cough syndrome
• Vocal cord dysfunction
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.
Occupational Asthma
Occupational factors probably account for 1 in 6 cases of asthma. It is more likely to develop in the first year of exposure and is often preceeded by work related rhinitis. Symptoms should improve away from work. If suspected, a referral to someone specialising in occupational asthma should be made.
Compensation for occupational asthma is a complex area but The Citizens Advice Bureau may offer advice about their eligibility for benefits and compensation.
National occupational asthma guidelines were published by the British Occupational Health Research Foundation (BOHRF), updated in 2010.
Subscribe to:
Comments (Atom)